Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 3
3 - Challenging Penicillin Allergies in Pediatric Patients
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 3
Publication Number: 3.3116
Publication Number: 3.3116

Alexandria Martin, MD (she/her/hers)
Resident
Madigan Army Medical Center
University Place, Washington, United States
Presenting Author(s)
Background: Antibiotics are the most common class of medication prescribed to children. Penicillin allergy labels are the primary reason pediatric patients are not treated with first-line antibiotic agents. Patients treated with alternatives are at higher risk of treatment failure and adverse reactions. Allergy labels are associated with prolonged hospitalizations, readmissions, and excess cost. Anywhere from 8-25% of patients carry a penicillin allergy label, but when challenged they are confirmed in < 3% of patients with reactions deemed low risk for an IgE-mediated or other serious reaction. Challenging and removing the penicillin allergy labels (“de-labeling”) is recommended. Generally de-labeling is done by allergists. However, there may be barriers to receiving specialty care and challenges performed outside of network may not lead to de-labeling within a local electronic medical record. A growing body of evidence supports primary care de-labeling when the prior reaction is deemed low risk.
Objective: Therefore, our team sought to establish a de-labeling process that may be performed within the pediatrics department.
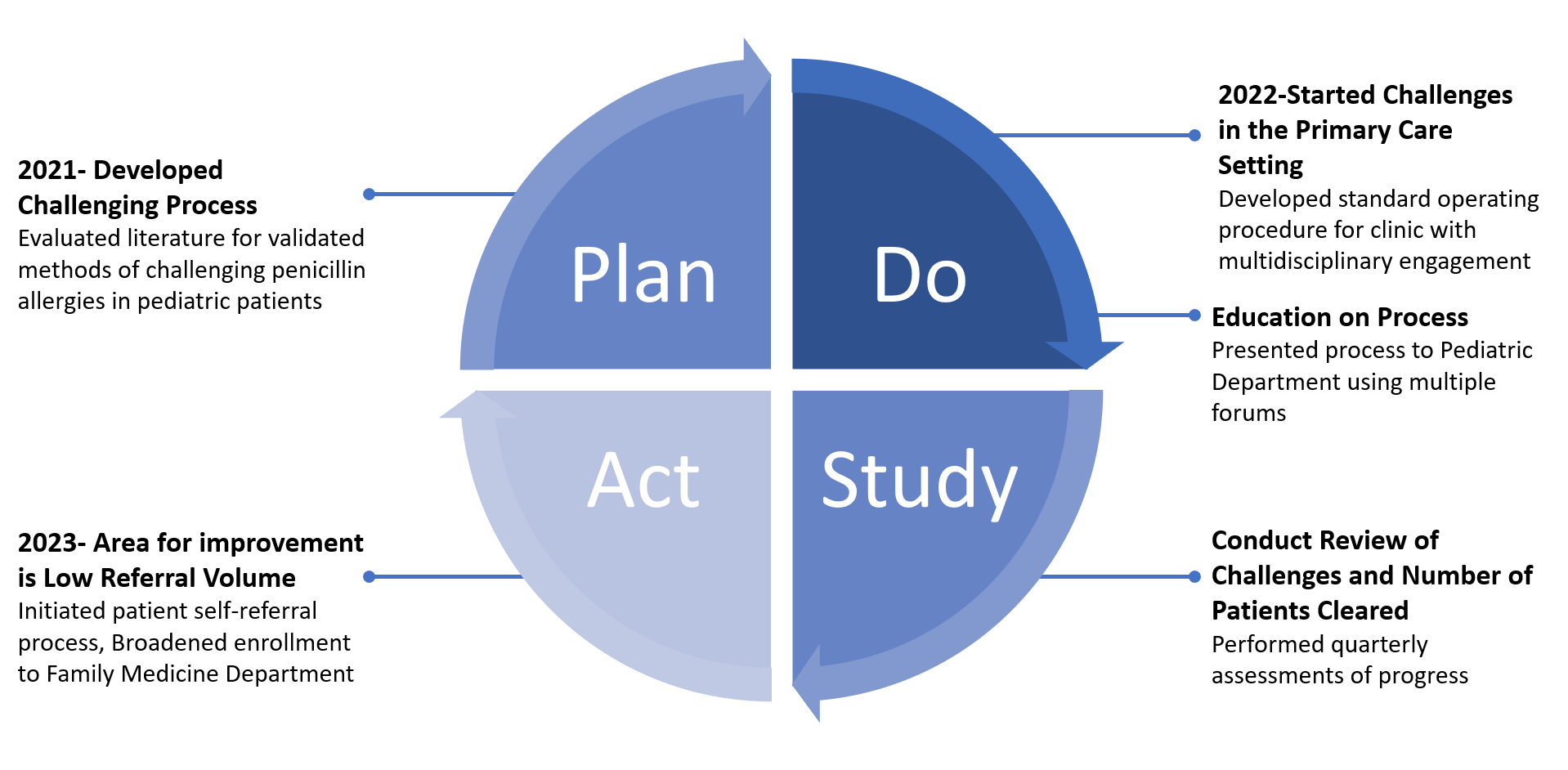
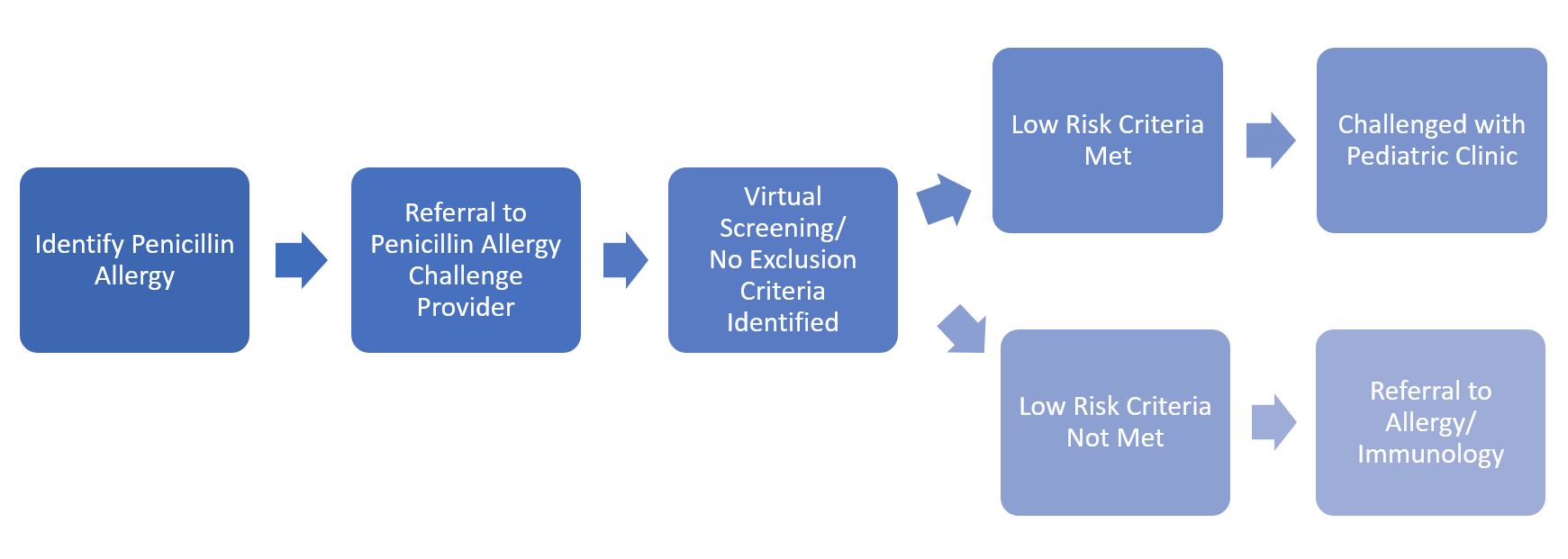
Design/Methods: Beginning in 2022, a multi-disciplinary team developed an evidence-based protocol to screen, challenge, and de-label pediatric patients with penicillin allergy labels(Figure 1). The team uses multiple modalities to advertise this project. When identified, eligible patients are referred for a virtual screening appointment(Figure 2). Only low risk reactions are challenged within the Pediatric Clinic; others are referred to Pediatric Allergists when indicated. All referrals that are deferred out of network for penicillin challenges are now recorded so results can be proactively obtained and rectified in our system.
Results: Thirty-seven patients have been referred for allergy de-labeling. Of 35 virtually screened to date, 2 were cleared based on history and 31 others were eligible for challenge. Twenty-one patients (68%) were stratified as low risk and therefore eligible for challenge by primary care. Fifteen have been successfully challenged and/or cleared, and 10 others are pending appointments. No adverse reactions have been reported.
Conclusion(s): The majority of pediatric patients who are referred for penicillin allergies are low risk for an IgE-mediated reaction and therefore can be safely challenged in primary care settings. This project meets a key objective of antibiotic stewardship while also modeling a de-labeling option that can be implemented in other resource-limited pediatric clinics.