Neonatology
Session: Neonatal Quality Improvement 6
96 - Standardizing Treatment of Necrotizing Enterocolitis in Infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 96
Publication Number: 96.3117
Publication Number: 96.3117

Amaris Lestinsky, MD (she/her/hers)
Resident Physician
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Necrotizing enterocolitis (NEC) is a life-threatening disease in high-risk newborns. Treatment involves bowel rest, gastric decompression, antimicrobial therapy and surgery in advanced stages of disease. There is inter-institutional and inter-provider variability in antibiotic selection, often involving Gram positive and negative coverage as well as anaerobic coverage in select cases. A standardized NEC treatment pathway was created in Aug. 2022 with an electronic order set to guide antibiotic selection for NEC in our institution.
Objective: The aim of this quality improvement project was to achieve 70% compliance with the NEC pathway from Aug. 2022 - Aug. 2023.
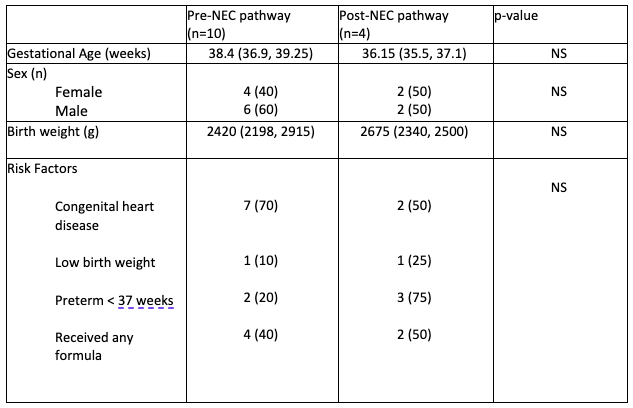
Design/Methods: For pre-pathway data, we reviewed NEC treatment from Jan. 2020- Dec. 2021. Pathway education occurred at monthly meetings with NICU, CVICU, PICU and surgery staff from Aug.- Dec. 2022. Collection of data is ongoing to track adherence.
Outcome measures: Percentage of appropriate antibiotic selection.
Process measures: Percentage of electronic order set use and use of a NEC dashboard.
Balancing measures: Rates of stage 3 NEC, surgical intervention, complications (strictures, abscess, wound dehiscence), and mortality rate.
Continuous variables were analyzed using paired t-test and categorical variables using Fisher’s exact test. A p-value < 0.05 was statistically significant.
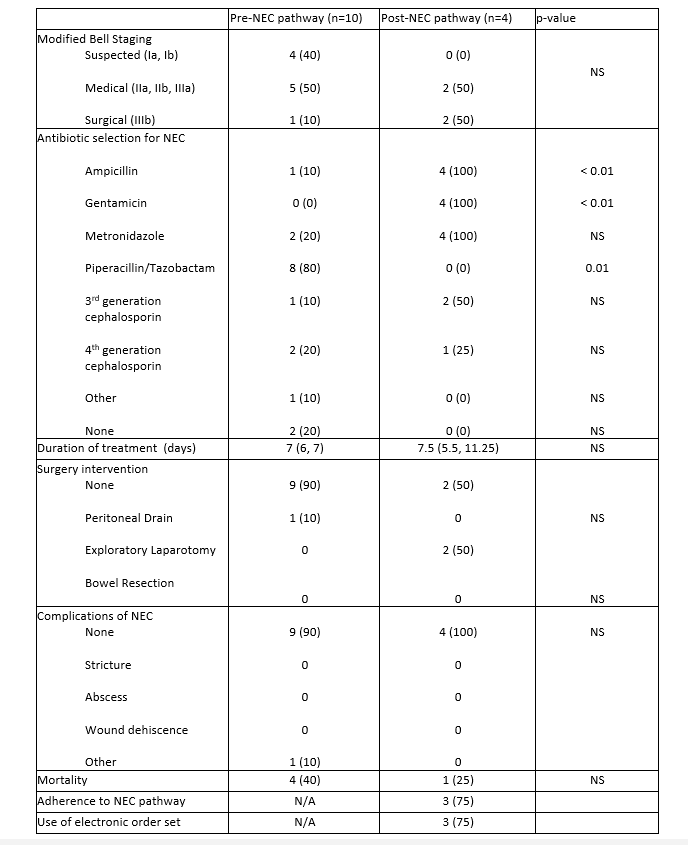
Results: Pre-pathway data was gathered from ten patients from Jan. 2020- Dec. 2021 (Table 1). 80% of NEC cases received piperacillin/tazobactam, 20% metronidazole and 10% cephalosporin (Table 2, Figure 1). Mortality occurred in 40% of cases.
Post-pathway data included four cases that were audited for NEC pathway compliance (Tables 1 and 2). Antibiotic selection favored ampicillin and gentamicin instead of piperacillin/tazobactam (p < 0.05) (Table 2, Figure 1). The electronic order set was used in 75% of cases.Two infants required surgical intervention. One baby died due to fulminant NEC upon transfer to the hospital (Table 2).
Conclusion(s): Pre-pathway, piperacillin-tazobactam was the antibiotic of choice for NEC at our institution. Post-pathway, four cases were audited. Use has shifted to ampicillin and gentamicin as per pathway recommendations (p < 0.01) without increases in mortality or higher stages of NEC. We achieved 75% adherence to electronic order set use in 1 year. A NEC dashboard allows for ongoing surveillance of NEC, antibiotic therapy selection, and use of the electronic order set.
.png)
