Medical Education
Session: Medical Education 5
407 - Evaluation of a Longitudinal Complex Care Curriculum
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 407
Publication Number: 407.1443
Publication Number: 407.1443

Joseph B. Wall, MD (he/him/his)
Resident House Doctor
NewYork-Presbyterian Morgan Stanley Children's Hospital
NEW YORK, New York, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) comprise a rising proportion of hospitalizations and healthcare costs. Providing effective care for CMC requires specialized knowledge and skills. Entrustable professional activities have been developed to guide training of pediatric residents, yet there are no standardized curricula. A few institutions have tried asynchronous modules or simulations with data supporting improved resident confidence in CMC care.
Objective: Assess the quality of the complex care curriculum and resident self-efficacy in caring for CMC through educational presentations.
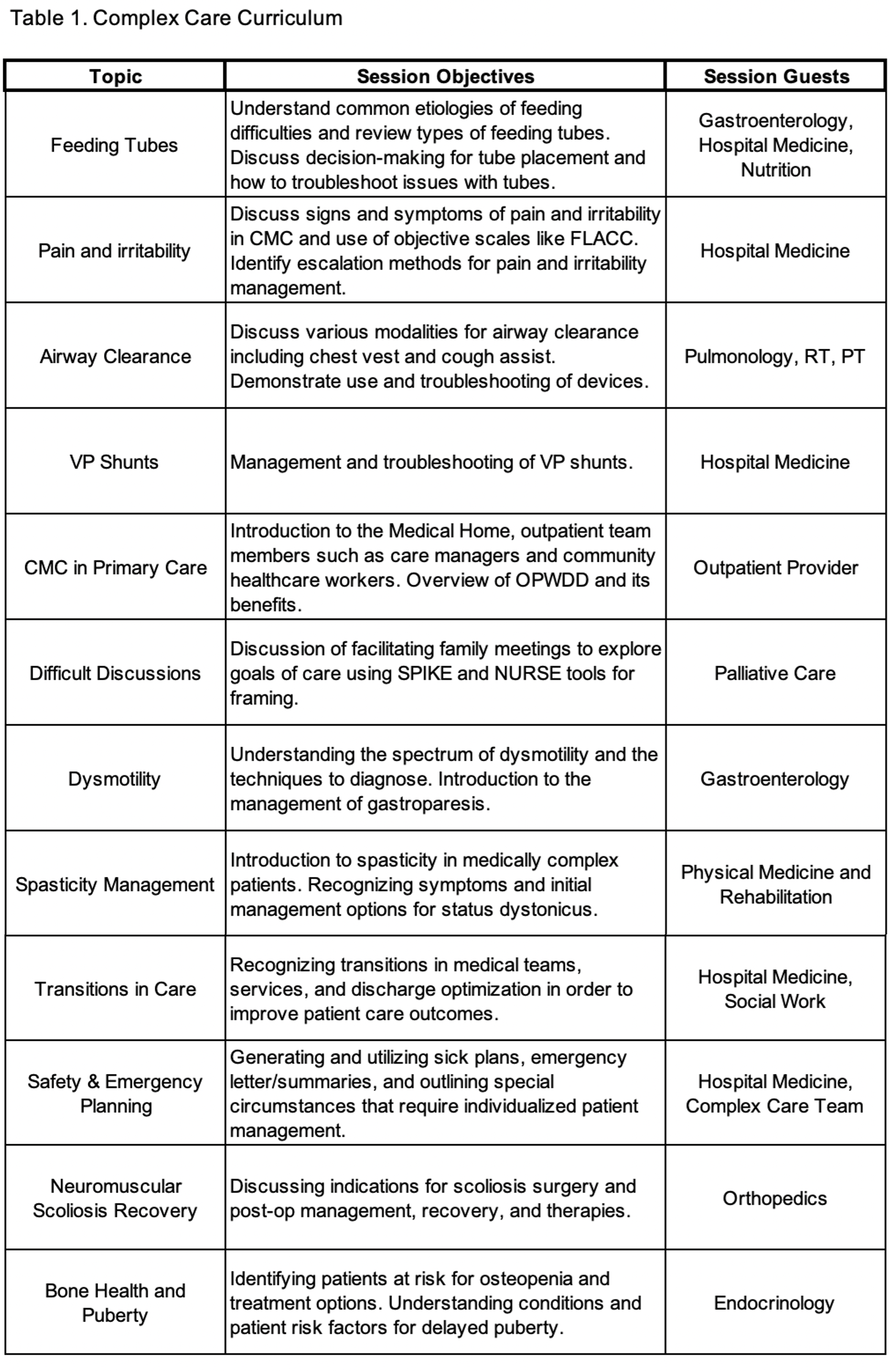
Design/Methods: The CMC curriculum was presented during resident conferences. Topics were selected based on a modified delphi study (K Huth et al), which highlighted curricular priorities in complex care (Table 1). Sessions were case-based, hands-on, and included medical technology. Multidisciplinary providers including subspecialists, respiratory therapists, and dieticians facilitated the sessions. Pediatric residents who attended completed a survey from the complex care team with retrospective pre-post questions and Likert scales. The survey results were used for curricular assessment, resident self-efficacy, and feedback. Data were analyzed using basic descriptive statistics and parametric analyses to compare the categorical data.
Results: Sixty-three surveys were completed for the twelve sessions. Residents responded favorably to prompts assessing the curriculum with an overall mean agreeing (35%) and strongly agreeing (63%) that the curriculum was important and appropriate (Table 2). Effectiveness of the curriculum was assessed based on resident self-efficacy from pre-post knowledge scales (Table 3). Due to some sessions having poor (N < 2) or no survey responses, a selection of the data is reported. It was found that resident self-efficacy increased with statistical significance across all objectives except for Difficult Discussions. These findings support the effectiveness of the curriculum in increasing resident self-efficacy.
Conclusion(s): A longitudinal complex care curriculum was found by the residents to be important, effective, and appropriate with an increase in self-efficacy. Development of a national standardized curriculum would benefit present and future pediatric physicians as all will encounter CMC in their practice. Limitations include response bias, lack of a control group and lack of long-term data assessing knowledge retention. Next steps are a qualitative analysis through interviews and further data collection to determine how or if the curriculum results in durable practice changes.
.png)
.png)
