Hypertension
Session: Hypertension
65 - Clinician Adherence to AAP Pediatric Hypertension Guidelines
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 65
Publication Number: 65.1919
Publication Number: 65.1919

Patrick Touhy, MD (he/him/his)
Physician/Academic Fellow
Wake Forest School of Medicine of Wake Forest Baptist Medical Center
Winston-Salem, North Carolina, United States
Presenting Author(s)
Background: Hypertension is a contributor to cardiovascular disease. In 2017, the American Academy of Pediatrics (AAP) released a complex clinical practice guideline (CPG) on diagnosis and management of hypertension. Knowing and following such recommendations may be challenging for pediatricians.
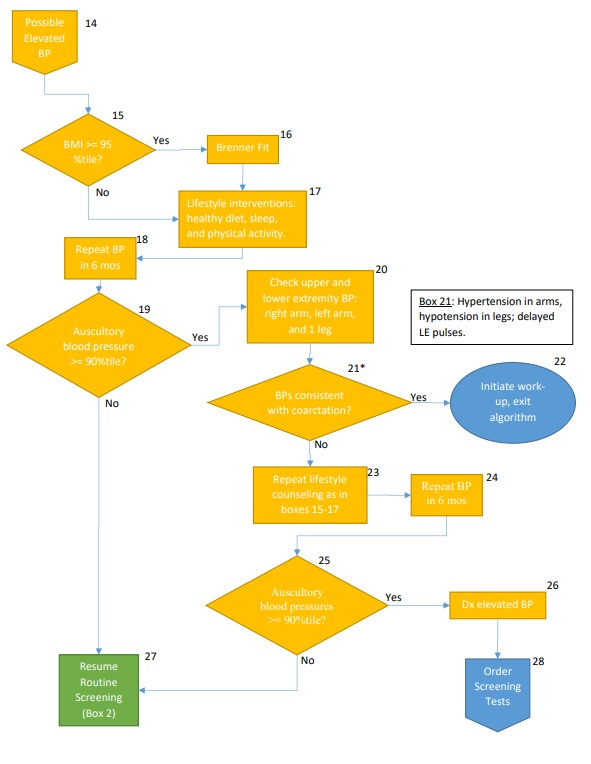
Objective: This project sought to assess changes in provider knowledge and adherence to key action statements regarding follow-up, evaluation, and treatment of hypertension from the 2017 AAP CPG after creating and implementing a decision-making algorithm (Figure 1) that follows the 2017 AAP CPG.
Design/Methods: This was a before-after comparison project that took place at an academic general outpatient pediatrics clinic. The study team created a novel decision-making algorithm that encoded recommendations from the 2017 AAP CPG. Pre-algorithm, a voluntary and anonymous knowledge assessment consisting of two multiple choice questions was given to all pediatric residents at Atrium Health Wake Forest Baptist (AHWFB). Questions asked about follow-up of abnormal blood pressure and management of hypertension. Additionally, patient data from the electronic health record (EHR) were pulled to assess adherence to the CPG during one year’s time at the study clinic. One year post-algorithm, the same knowledge assessment was given to all pediatric residents at AHWFB. Similarly, patient data were collected from the EHR to assess provider adherence for the year following installation of the algorithm. Chi squared tests were utilized, in addition to descriptive statistics, to analyze the data pre/post –algorithm.
Results: Pre-algorithm, 78% of residents completed the knowledge assessment. None of them answered both assessment questions correctly. 62% of residents completed the post-algorithm knowledge assessment. Post-algorithm, 7% answered both assessment questions correctly. This was not a significant change (Table 1). When comparing EHR data pre/post-algorithm, however, there was a significant increase in appropriate patient repeat blood pressure measurements amongst patients with abnormal blood pressure measurements (Table 1).
Conclusion(s): Although limited by size, this project showed poor clinician knowledge of the 2017 AAP CPG that was not significantly improved with the availability of an evidence-based decision-making algorithm. Nonetheless, a significant increase in patient follow-up, and thus, overall care of patients with abnormal blood pressure measurements was observed. This argues that use of such an algorithm can improve hypertension care, and similar tools may benefit other areas of pediatric care with complex CPGs.
.jpg)
