Children with Chronic Conditions
Session: Children with Chronic Conditions 1
262 - Post-traumatic stress disorder in parents of children with medical complexity: prevalence and associations
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 262
Publication Number: 262.292
Publication Number: 262.292

Tammie Dewan, MD, MSc (she/her/hers)
Pediatrician
Alberta Children's Hospital, University of Calgary
Calgary, Alberta, Canada
Presenting Author(s)
Background: Parents of children with medical complexity (CMC) are repeatedly exposed to high levels of stress including difficult diagnoses, critical illness and challenging healthcare encounters. These experiences place them at risk of post-traumatic stress disorder (PTSD).
Objective: (1) To determine the prevalence of PTSD in parents of CMC;(2) To describe relevant associations with parent/child characteristics and parent experiences of hospital care.
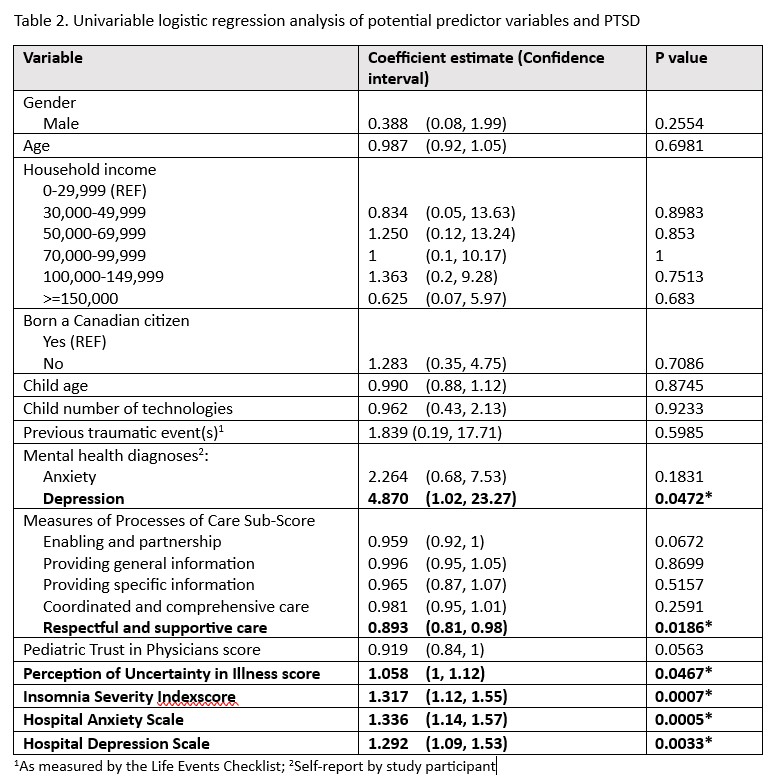
Design/Methods: In this cross-sectional study, parents of CMC were enrolled during their child’s hospital admission. Symptoms of PTSD were measured using the Posttraumatic Stress Checklist (PCL-5) with a cutoff of 33 points out of 80 indicating probable PTSD. Relevant demographic (parent/child) and child illness variables were collected as well as parent-reported measures of experience of care (illness uncertainty, trust, patient-centeredness of care, depression, anxiety, sleep).Univariable logistic regression was used to identify significant associations between these variables and PTSD.
Results: In total, 75 participants were enrolled from 12/2021 and 05/2023 and 63 completed survey data. Mean age of parents was 39.7 (8.61) years and 75% were female. Almost one-third had a household income less than $70,000/year and 29% were born outside of Canada. The children had a mean age of 6.7 (4.8) yrs and 60% had a neurodevelopmental disorder. At baseline, 18/63 or 28.6% of parents met criteria for probable PTSD based on PCL-5 score. Probability of PTSD was associated with parent-reported diagnosis of depression and parent ratings of current depression/anxiety symptoms, uncertainty (measured by Parental Perceptions of Illness Uncertainty scale), parental insomnia (measured by the Insomnia Severity Index) and parental ratings of respectful/supportive care on the Measures of Processes of Care. No association was found between PTSD and parent/child gender, child characteristics (age, technology, developmental disability), whether the child required PICU during that admission or lifetime traumatic events.
Conclusion(s): The prevalence of PTSD is significantly higher in parents of CMC compared to many other childhood chronic/critical illnesses. PTSD is significantly associated with poor parental sleep and parental anxiety/depression. There was no association found between PTSD and indicators of greater child fragility/complexity. Parents with PTSD rated their experiences of hospital care significantly worse in certain areas. In particular, they report greater uncertainty in their child’s illness and perceive care as less respectful/supportive.
.jpg)