Neonatology
Session: Neonatal Nephrology/AKI 1
44 - The ANCHOR Fluid Balance Calculator: Development and pilot testing of a novel fluid calculator for use in infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 44
Publication Number: 44.1926
Publication Number: 44.1926

Jennifer L. Chmielewski, MD (she/her/hers)
Neonatology Fellow
Indiana University School of Medicine
Westfield, Indiana, United States
Presenting Author(s)
Background: Fluid overload, defined as a state of pathologic fluid excess or positive fluid balance, is increasingly recognized as a deleterious state in critically ill infants. Assessing fluid balance is further complicated in critically ill infants when accounting for expected growth. There is a lack of consensus on how to best assess fluid balance once infants return to their birth weight.
Objective: To develop and pilot test a fluid balance calculator for use in infants after return to birth weight, accounting for expected weight gain. We hypothesize that such a fluid calculator is a feasible method of assessing fluid balance and would be clinically useful.
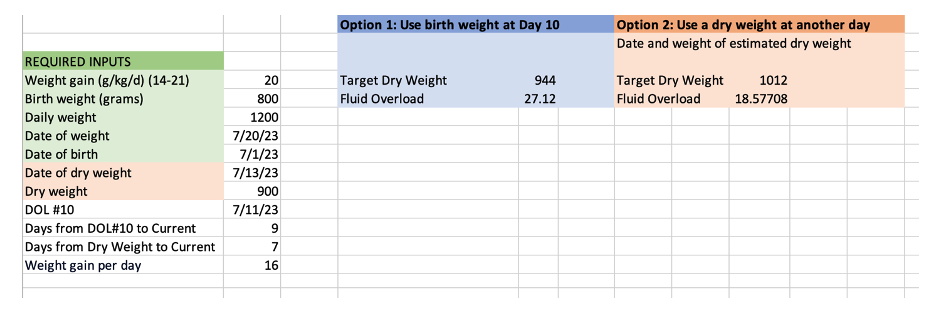
Design/Methods: Through an iterative process, we first developed and refined the ANCHOR fluid balance calculator (Assessing Newborn Change in weigHt and fluid Overload Rapidly). Based on previous studies, we estimated return to birth weight at day 10. Required information includes birth weight, expected daily weight gain (ranging from 14-21g/kg/day, which was standardly set to 20), and daily weight (Fig1). For infants >100 days, an estimated euvolemic or anchor weight was optional but recommended to improve the calculator output. We first pilot tested the ANCHOR calculator on infants in a small single-center bronchopulmonary dysplasia (BPD) cohort and then on a small subset of the multi-center PENUT cohort.
Results: In 37 infants with BPD (ranging 23-32 weeks gestation and 14-153 days old) from our pilot testing cohort, the ANCHOR Calculator quickly and easily calculated fluid balance. Fluid balance ranged from -2% to 39%. In the 14 patients with fluid balance >20%, 71% (10/14) were noted to be either fluid overloaded or edematous within the last week based on clinical notes.
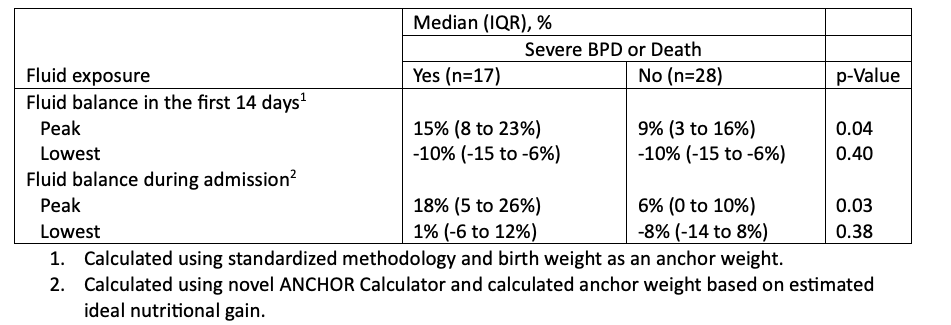
In 45 randomly selected infants from the PENUT cohort, we assessed fluid balance using the ANCHOR calculator and associations with a composite of severe BPD or death. Severe BPD or death was associated with peak fluid balance during admission (median 18% above calculated anchor weight vs 6% above calculated anchor weight among those with mild or no BPD (P=0.03)) (Table1).
Conclusion(s): We describe the development and pilot testing of a novel fluid balance calculator to determine fluid balance in infants after return to birth weight. Our pilot testing shows that such a tool is clinically feasible and useful. Use in a small subset of premature infants shows strong association with clinically relevant pulmonary outcomes. Such a tool will soon be available free and open-access as a online fluid calculator. Further work is needed to refine the tool with a plan for multicenter validation.