Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 8
324 - The relationship between levels of neighborhood opportunity and mental health and developmental disabilities diagnoses for children in an urban area
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 324
Publication Number: 324.1932
Publication Number: 324.1932

Deborah W. Davis, PhD (she/her/hers)
Professor
University of Louisville School of Medicine
Louisville, Kentucky, United States
Presenting Author(s)
Background: Disparities in childhood health and development have been found across domains. The role of racism, including neighborhood disadvantage, has been described for adults and some childhood conditions. The role of racism in the diagnosis of childhood mental health (MH) and developmental disabilities (DD) diagnosis has been less well described.
Objective: Describe the distribution of MH and DD diagnosis across Child Opportunity Index (COI) levels by race/ethnicity for a sample of children ages 0-17 years.
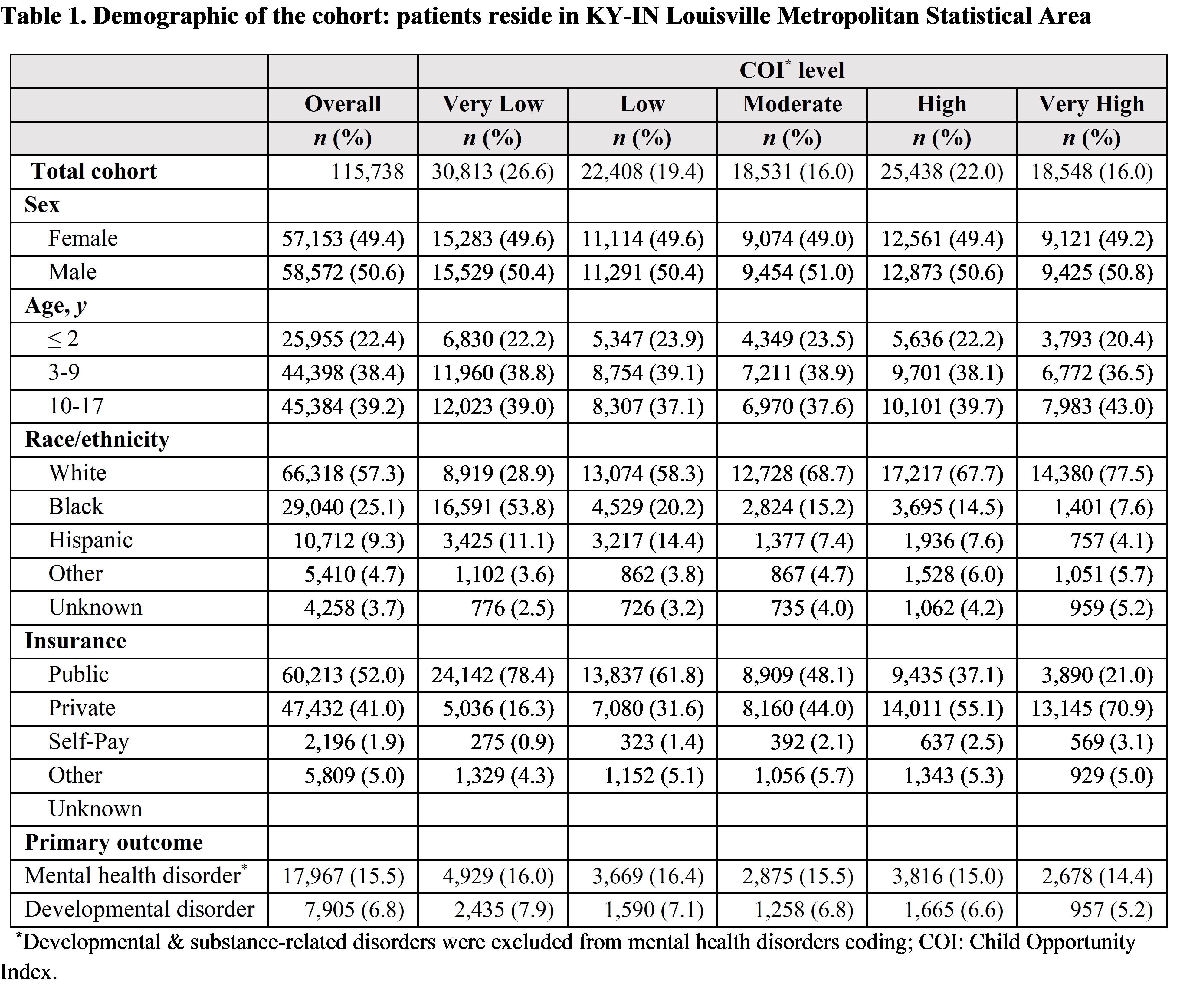
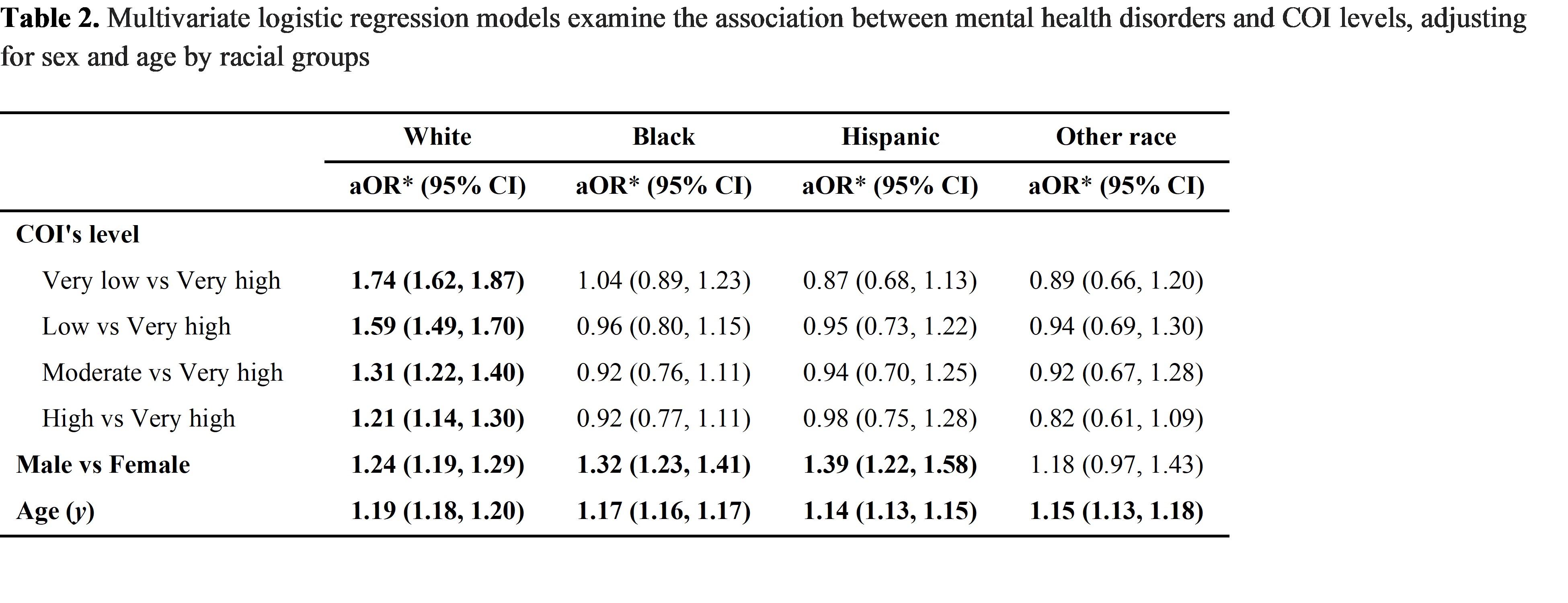
Design/Methods: This is a cross-sectional analysis of outpatient visit data in 2022 from a large children’s health system (n=181,887). Children < 18 years of age with valid addresses living in the KY-IN Louisville Metropolitan Statistical Area (CBSA 31140) were included (n=115,738). The primary independent variable was child opportunity levels (from “very low” to “very high”), as defined by the 2015 metro-normed COI 2.0. Home addresses were geocoded and linked by census tract in the KY-IN Louisville Metropolitan Statistical Area. Our outcome was MH diagnosis (excluding DD and substance-use disorders) and DD. Multivariate logistic regression models were performed to examine the association between diagnoses and COI levels, controlling for child sex and age.
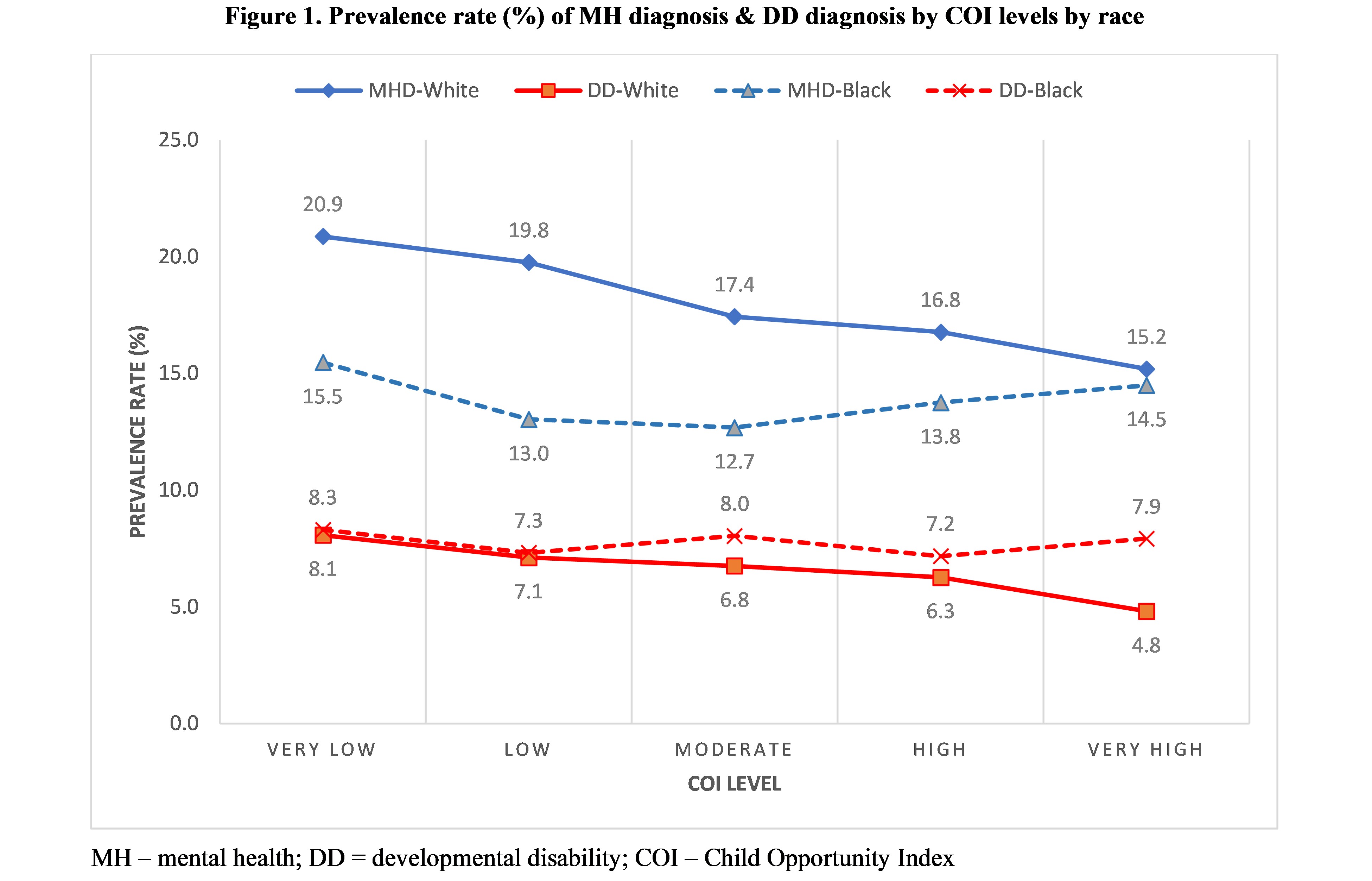
Results: Almost 18,000 children (15.5%) had a MH diagnosis and 7,905 (6.8%) had a DD (Table 1). The prevalence rate of MH diagnosis was lower for non-Hispanic (N-H) Black children than for N-H White children in each COI level (Figure 1). DD were diagnosed slightly less for N-H White children than N-H Black children. In multivariable logistic regression, COI was associated with MH diagnosis for N-H White children only (Table 2) with an aOR (95% CI) of receiving a MH diagnosis for children living in a Very Low compared to a Very High COI area of 1.74 (1.62, 1.87). Similarly, for N-H White children only, the aOR (95% CI) of receiving a DD diagnosis for children living in a Very Low compared to a Very High COI area was 1.69 (1.51, 1.88; not shown). There were no significant associations between diagnoses and COI for children who were N-H Black, Hispanic, or Other race/ethnicity for MH or DD diagnoses.
Conclusion(s): The current findings suggest that COI, which may be a proxy for access to care does not explain disparities in diagnosis for non-White children. More research is needed to identify root causes such as provider bias, caregivers’ medical mistrust, and other potential forms of interpersonal and structural racism. Additionally, identification of protective factors may inform interventions.