Medical Education
Session: Medical Education 8
484 - A Resident-Led Quality Improvement Initiative to Improve Trainee Confidence in Clinical Breastfeeding Support
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 484
Publication Number: 484.3089
Publication Number: 484.3089

Claire Gallibois, MB, BCh, BAO (she/her/hers)
Neonatology Fellow
Medstar Georgetown University Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Pediatric residents are often the primary providers for infants, thus their knowledge on breastfeeding principles is critical to counselling breastfeeding parents confidently. However, literature suggests that most residents lack comfort in this area. Pediatric residents at our hospital identified knowledge gaps around breastfeeding owing to a lack of structured breastfeeding education.
Objective: As part of an experiential pediatric residency quality improvement (QI) curriculum, we developed a breastfeeding curriculum focused on incorporation of structured breastfeeding didactics and dedicated time with lactation consultants into our residency education. The specific aims were 1) improve resident attendance of clinical experiences with lactation by 25% and 2) improve knowledge and confidence in breastfeeding counselling by 25%, over a 9-month period.
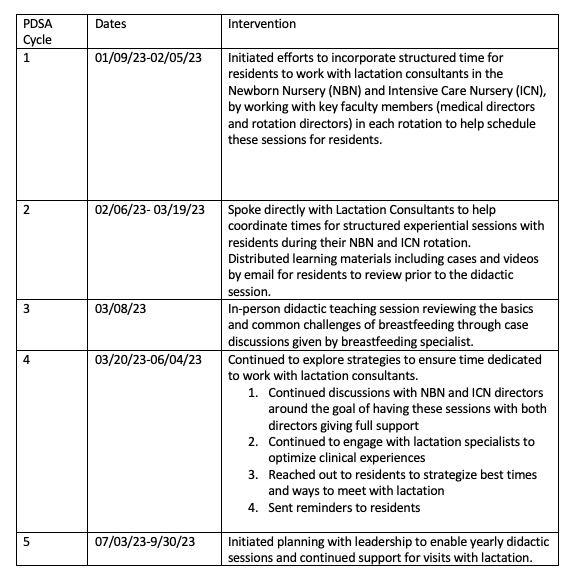
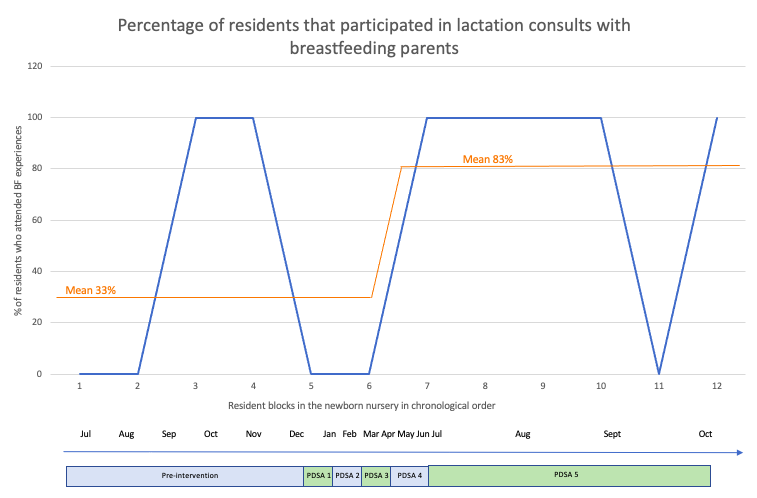
Design/Methods: A resident-led team applied the Institute for Healthcare Improvement’s Model for Improvement to execute 5 Plan-Do-Study-Act (PDSA) cycles (Table 1). We worked with local teams to ensure all residents had dedicated time on their newborn nursery rotation to participate in visits with lactation consultants. We also incorporated a didactic teaching session for residents facilitated by a breastfeeding specialist. Baseline data was collected from 09/22-12/22, active improvement took place from 01/23-06/23, and sustainability continued from 07/23-09/23. Our primary process measure was resident participation in lactation consults during their newborn nursery rotation. The results of the pre- and post-didactic surveys, which assessed residents’ knowledge of breastfeeding principles and confidence in counselling, were the outcome measures.
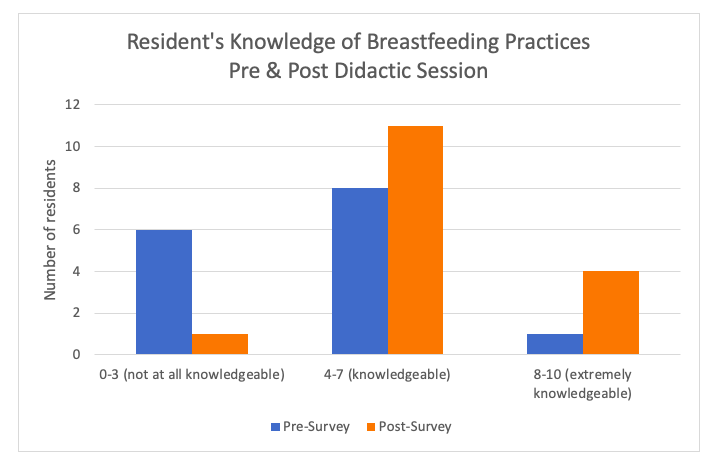
Results: Surveys were sent to 15 residents; response rates were 100% for the pre- and 60% for the post-survey. Correct answers to the knowledge questions increased from 65% to 71% (p=0.21) from the pre-to-post surveys (Figure 1), while confidence in breastfeeding counselling increased from 42% to 66% (p=0.19). Resident attendance at lactation visits increased from a mean of 33% to 83% (Figure 2).
Conclusion(s): This resident-led, collaborative QI intervention successfully increased experiential lactation consultation involvement for pediatric residents. Confidence and knowledge relevant to counselling improved as well, but improvement failed to meet our specific aims. Active involvement of the breastfeeding specialist and lactation consultants were essential to the success of the breastfeeding curriculum while barriers included inconsistent resident participation and changes in leadership.