Emergency Medicine
Session: Emergency Medicine 9: Respiratory
227 - Trends and Disparities in Asthma Admission from the Pediatric Emergency Department
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 227
Publication Number: 227.3091
Publication Number: 227.3091
- LS
Laura Sartori, MD, MPH
Assistant Professor
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Asthma is a common and well-studied reason for presentation to the Pediatric Emergency Department (ED). Despite decades of advancement in evidence-based care, variation exists in pediatric asthma admission rates. Racial disparities in asthma care, including steroid administration and chest x-ray performance, have been identified, but potential disparities in asthma admission are less well understood.
Objective: To examine trends in asthma admission rates over time, including variation in admission rates by patient race and ethnicity.
Design/Methods: We analyzed acuity-adjusted asthma admission rates for all children presenting to the ED with acute asthma exacerbation from 2018-2023 at a single tertiary care children’s hospital. Average admission rates weighted by 2022-23 triage acuity distribution were calculated by year and stratified by patient race and ethnicity as designated in the electronic health record (EHR). We examined return visits to the ED within 72 hours as a balancing measure. Trends were analyzed by fiscal year using descriptive statistics and logistic regression.
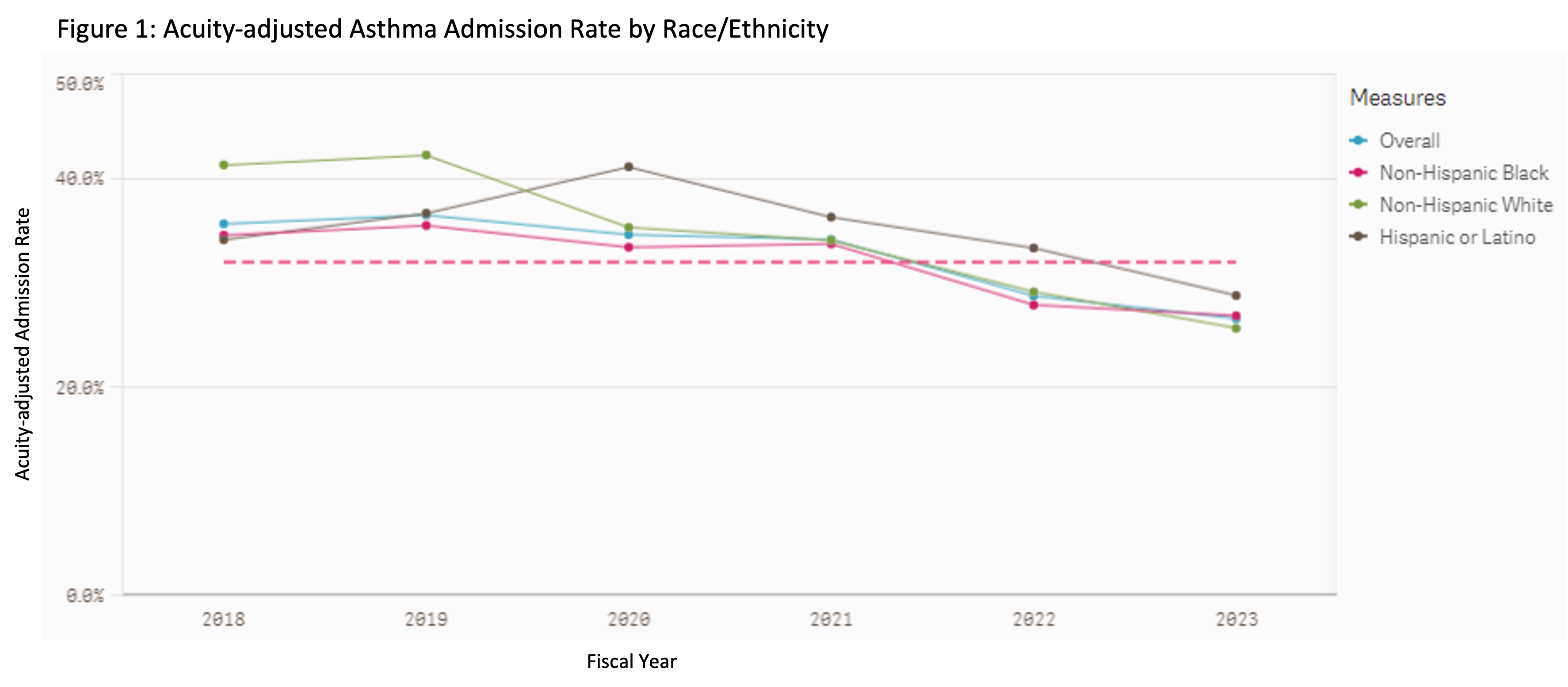
Results: A total of 33,776 ED asthma encounters were analyzed, with substantial decreases in asthma visits during the pandemic period of 2020-21. 70.9% of patients were categorized as Non-Hispanic Black (NHBlack). Acuity-adjusted asthma admission rates decreased over the study period (35.7% in 2018 vs. 26.6% in 2023, p< 0.001, see Figure 1.). Prior to the pandemic in 2018-19, acuity-adjusted admission rates were significantly higher for Non-Hispanic White (NHWhite) compared to NHBlack patients (42.0% vs 35.2%, p< 0.001). This difference decreased during 2020, and rates have been similar in the post-pandemic period. Hispanic/Latino patients had higher admit rates across the study period compared to NHBlack patients (p < 0.001). ED asthma revisit overall and by race/ethnicity category did not change significantly over the study period (Figure 2).
Conclusion(s): Admission rates for asthma have decreased over time without associated increases in revisits. Disparities in admission rates have also decreased since the pandemic. Interventions during this time-period included standardized EHR decision support and reporting disparities to the faculty group. Though we hypothesize that some of these changes were driven by reduced hospital capacity, particularly during the viral surge period, the sustained decreased admission and disparity reduction since resolution of the pandemic warrants further investigation, including qualitative assessments of provider disposition decision-making.
.jpg)
