Neonatology
Session: Neonatal Quality Improvement 4
61 - Improving Neonatal Antibiotic Administration Timeliness in a Large Regional Quality Improvement Collaborative
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 61
Publication Number: 61.3084
Publication Number: 61.3084

Meghali Singhal, MD
Medical Director
Pediatrix
Sugar Land, Texas, United States
Presenting Author(s)
Background: Neonatal sepsis is a leading cause of infant morbidity and mortality. The timely initiation of antibiotics potentially improves patient survival. A mission of the Southeast Texas Regional Advisory Council (SETRAC) Perinatal Committee is to improve health outcomes of neonatal patients within our region encompassing approximately 50,000 births in 38 neonatal intensive care units (NICU). Improving initial empiric antibiotic timeliness in NICU admits was the focus of this committee project.
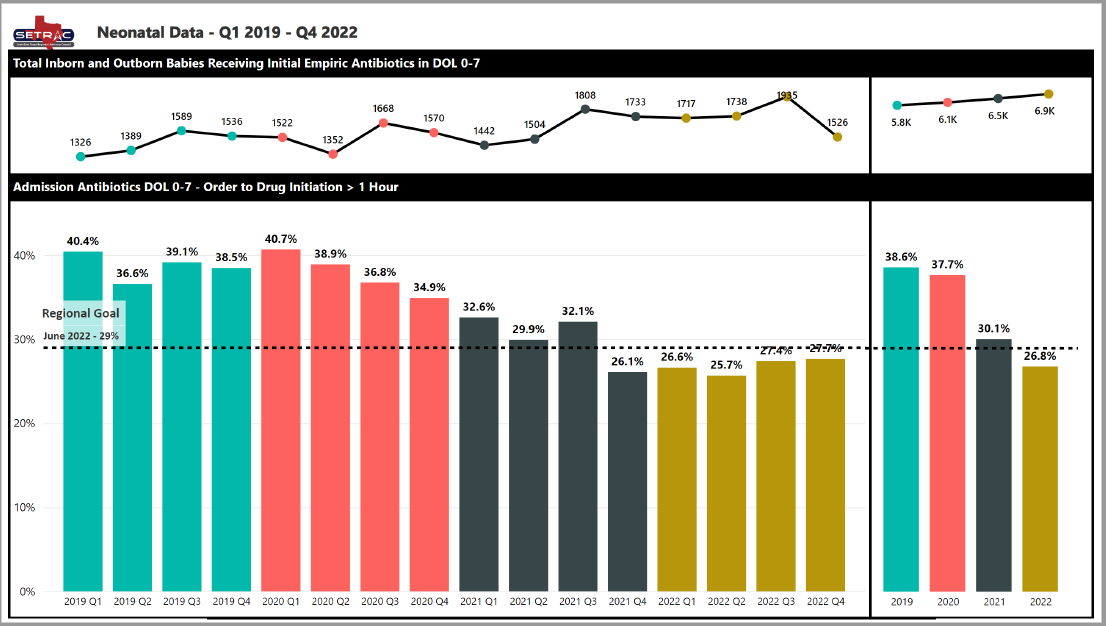
Objective: After initial data collection from January 2019 to December 2020, the goal of this project was to decrease the percentage of patients receiving antibiotics between day of life (DOL) 0 to 7 greater than 60 minutes after order/birth from 41% to 31% by June 2022.
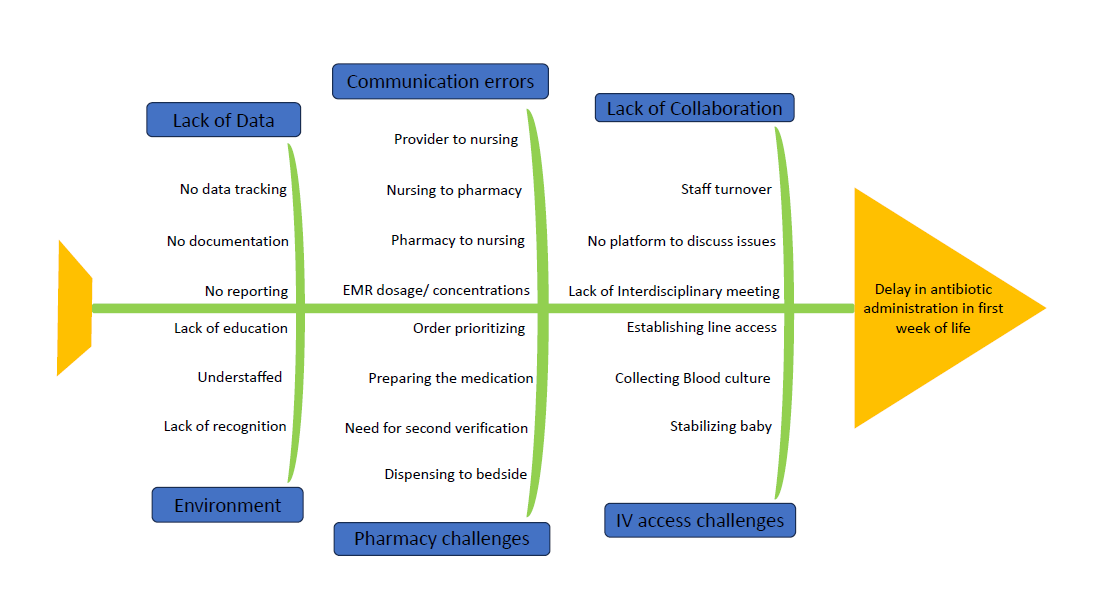
Design/Methods: A quality improvement project was initiated using a multidisciplinary team of neonatal providers within the SETRAC Perinatal Committee to improve rates of antibiotic timeliness in the first week of life. Recurring meetings and surveys with participation from multidisciplinary teams across Southeast Texas were utilized to identify the root causes of delay and common challenges faced by NICUs to improve timely antibiotic administration. Discussions led to the creation of a web-based toolkit intervention (found at www.setrac.org/perinatal under the “Antibiotic Timeliness Toolkit”) to provide resources and guidance to programs to improve antibiotic timeliness. Numerous Plan-Do-Study-Act (PDSA) cycles occurred. Key outcomes included total number of NICU patients who received any antibiotic between DOL 0 to 7 and percent of antibiotics where order to drug initiation was greater than 60 minutes.
Results: Prior to the intervention, the percent of administered antibiotics in NICU infants on DOL 0 to 7 greater than 60 minutes after order/birth was 38.6% (n=5800) in 2019 and 37.8% (n=6100) in 2020. After the interventions, the percent of antibiotic administration greater than 60 minutes decreased to 30.2% (n=6500) in 2021 and decreased further to 26.9% (n=6900) in 2022.
Conclusion(s): The percent of neonates receiving antibiotics greater than 60 minutes after order or birth greatly decreased through collaborative QI within the SETRAC Perinatal Committee. The development of a web-based toolkit, multiple PDSA cycles, and open discussion within a multidisciplinary team facilitated improvements in patient care through a large-scale quality improvement project. A massive improvement in key quality measures is possible through regional QI collaborative participation.