Neonatology
Session: Neonatal Quality Improvement 4
64 - Navigating Long-Term Mechanical Ventilation (LTMV) for Children with Chronic Respiratory Failure (CRF): Insights from Parents and Healthcare Providers
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 64
Publication Number: 64.3082
Publication Number: 64.3082
.jpg)
Amit Agarwal, MD (he/him/his)
Professor of Pediatrics
University of Arkansas for Medical Sciences College of Medicine
Little Rock, Arkansas, United States
Presenting Author(s)
Background: While impactful, initiating LTMV in children with CRF leaves families and healthcare providers with difficult choices. Hence, this requires a collaborative shared decision-making process (SDM) between parents and providers. There is scant literature about the informational needs of the family or provider perspectives.
Objective: To investigate (a) the informational needs of families and (b) the perspectives of providers involved in SDM for initiating LTMV.
Design/Methods: To aid providers who assist families in SDM,14 parents across 8 families who faced decisions around LMTV for their child were interviewed. The parental needs and experiences related to informed decision-making were assessed. An iterative process was utilized to develop a semi-structured interview with open-ended questions based on published literature and clinical experience. Interviews were then conducted via video conferencing. Additionally, 25 providers, including physicians and ancillary staff, were interviewed to evaluate how they facilitate SDM around LTMV, emphasizing the family’s decisional needs. A qualitative data analysis approach was utilized using a thematic approach based on framework analysis with the goal of thematic saturation.
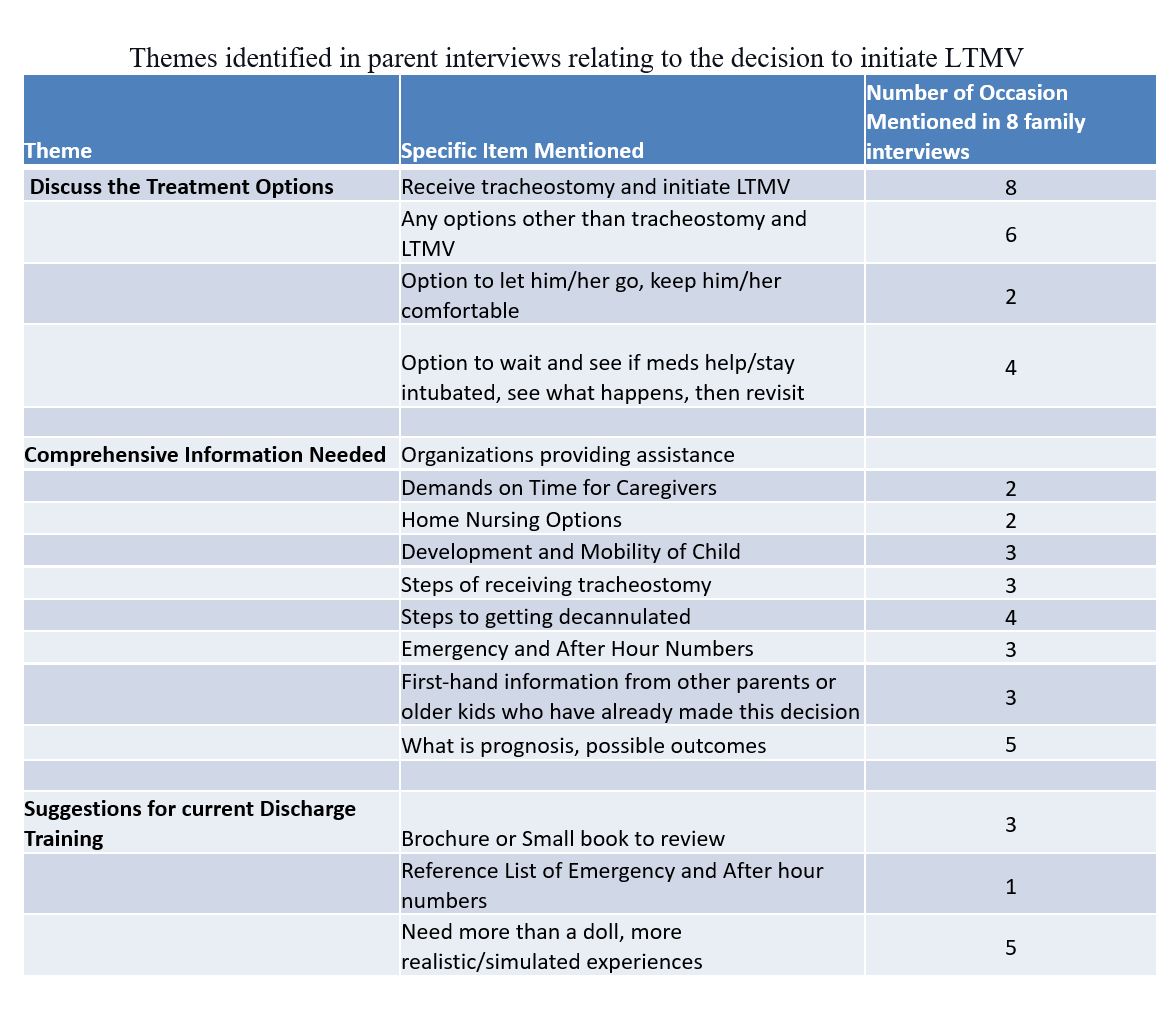
Results: All parents favored choosing LTMV for their child. Most parents reported that the decision process for LTMV was stressful. Some wished that they had been engaged earlier in the discussion and wanted comprehensive information (Table). Parents also felt it was acceptable to be presented with the option not to initiate LTMV.
Most providers interviewed recommended that decision-making around LTMV be interdisciplinary and initiated as soon as CRF is anticipated or diagnosed. Many echoed the need for multiple small group meetings to discuss the child’s progress and a checklist approach for conducting SDM meetings. Most participants recommended that providers be transparent, candid, supportive, and active listeners. Parents also mentioned that providers should inquire about the family goals and values and address whether LTMV can help achieve these goals. Several providers and parents emphasized the importance of early discharge training and improving the methods involved.
Conclusion(s): All stakeholders favored the SDM process for initiating LTMV. Parents called for comprehensive, unbiased, and early discussions around the burdens, risks, and benefits of LTMV. Providers supported standardization of the SDM processes, and all favored improving the multidisciplinary hospital-to-home transition training. We are piloting a quality initiative to improve the care of these children at our hospital.