Neonatology
Session: Neonatal Infectious Diseases/Immunology 2
606 - Epidemiology and Outcomes of Multidrug-Resistant sepsis in the Neonatal Intensive Care Unit: A National Cohort Study
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 606
Publication Number: 606.318
Publication Number: 606.318
Joseph Ting, MD, MPH
Associate Professor
University of Alberta
Edmonton, Alberta, Canada
Presenting Author(s)
Background: Neonatal sepsis is associated with increased mortality, morbidity, and healthcare expenditures. Increasing multi-drug resistance (MDR) has been a global concern, however, there exists a dearth of population-based studies elucidating its impact on neonatal outcomes.
Objective: To identify the incidence of MDR organisms during the first episode of neonatal sepsis and compare neonatal outcomes of those with and without MDR sepsis
Design/Methods: We utilized the Canadian Neonatal Network database platform for very-low-birth-weight infants (VLBW, birth weight < 1500g) admitted between Jan 2021-Dec 2022. MDR Gram-positive cocci included either methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant S. aureus (VRSA), or vancomycin-resistant Enterococcus (VRE). MDR Gram-negative bacilli were defined as those resistant to third-generation cephalosporin (3GC). Sepsis was defined by the isolation of a pathogen from blood and/or cerebrospinal fluid. The composite primary outcome refers to mortality or major morbidity, defined as the presence of any of the following: periventricular leukomalacia, retinopathy of prematurity ≥stage 3, necrotizing enterocolitis ≥stage 2, or bronchopulmonary dysplasia. Rates of individual morbidities were also compared. Adjusted odds ratio (AOR) for outcomes were calculated after controlling for sex and SNAPII score.
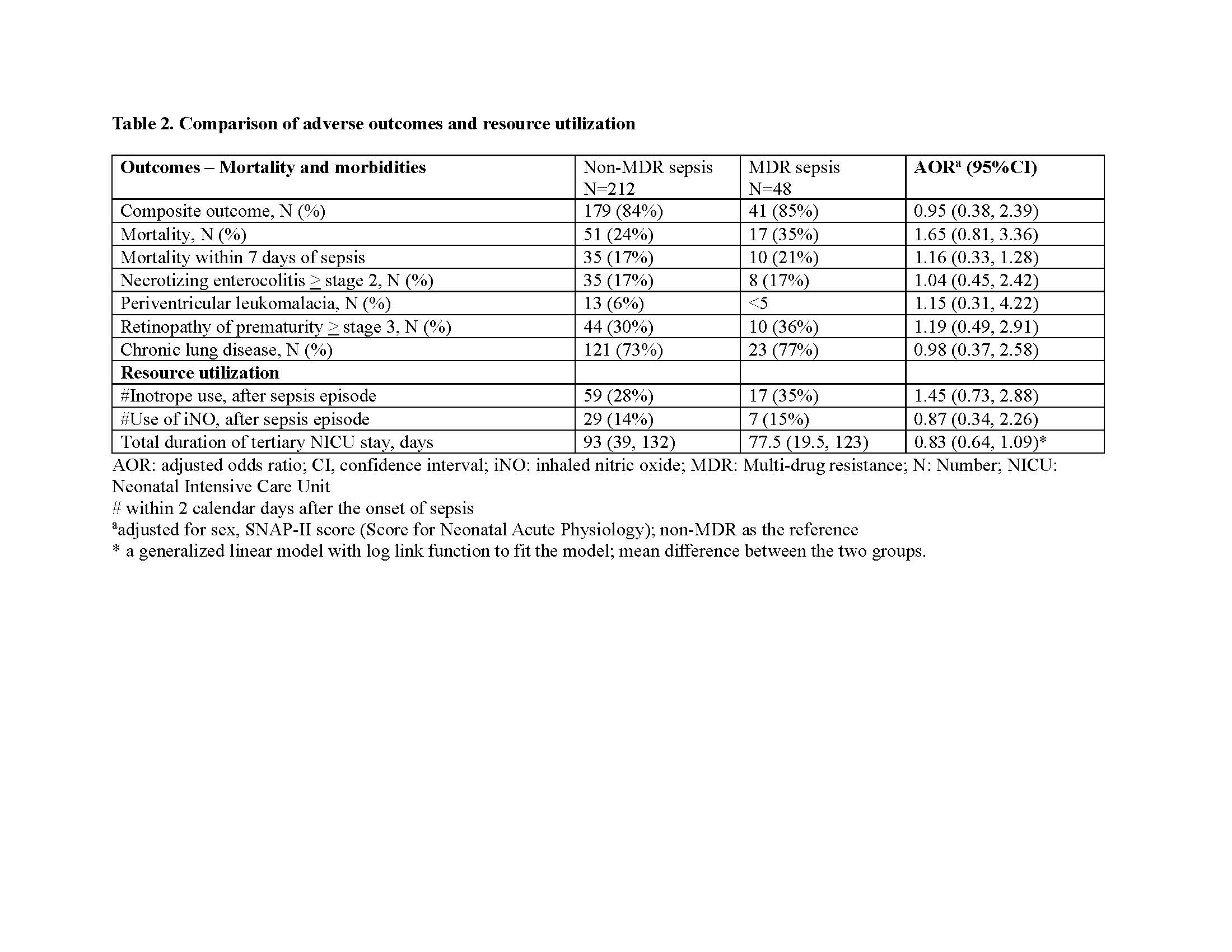
Results: We identified 88 infants with S. aureus sepsis, 124 with E coli sepsis, 40 with Klebsiella sepsis, and 8 infants with sepsis due to other MDR species [Table 1]. No strains of VRSA, VRE, or Carbapenamase-resistant bacteria were reported. Of these 10 (11.4%) of S. aureus isolates were MRSA; 22 (17.7%) of E. Coli and 8 (20%) of Klebsiella isolates had resistance to 3GC. No significant variations in demographic variables, duration of parenteral nutrition, length of mechanical ventilation, or prior exposure to 3GC were identified in infants with and without MDR sepsis [Table 1]. No differences were noted in adverse composite outcomes, mortality or individual morbidity [Table 2]. Subgroup analysis revealed increased mortality amongst MRSA as opposed to non-MRSA isolates, with an adjusted odds ratio of 7.11 (95% CI [1.63, 31.08]).
Conclusion(s): One in six bacterial isolates responsible for neonatal sepsis were caused by MDR organisms in our cohort. There were no significant differences in the composite outcomes of mortality and major morbidity between MDR and non-MDR sepsis. However, MRSA sepsis may be associated with higher odds of mortality compared to sepsis from methicillin-susceptible S. aureus strains.
.jpg)
