Infectious Diseases
Session: Infectious Diseases 3
135 - Utilizing penicillin administration data to assess the incidence and reporting of congenital syphilis cases in a tertiary children’s hospital in Chicago, Illinois
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 135
Publication Number: 135.1950
Publication Number: 135.1950

Yeo Won Ahn, MD (she/her/hers)
Pediatric Resident
Comer Children's Hospital at University of Chicago Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background: Congenital syphilis (CS) cases are increasing in the US. Definitive diagnosis is unusual, requiring spirochete identification using darkfield microscopy. More commonly, cases are classified as highly probable, possible, less likely or unlikely based on interpretation of nontreponemal serologic titers, adequacy of maternal treatment, and other clinical, laboratory, and radiographic findings. Consequently, accurate identification of CS can be challenging and lead to inconsistent reporting. The treatment of CS is penicillin, an antibiotic rarely indicated in neonatal infections other than Group B Streptococcus, and its administration data could be a useful supplemental measure of CS cases.
Objective: To utilize penicillin administration as an alternative method for identification of infants with clinical concern for CS to assess the incidence of and improve the reporting of CS.
Design/Methods: We extracted pharmaceutical data on patients who received parenteral penicillin in 2011-2022 at a children’s hospital in Illinois and audited patient records for therapeutic indication.
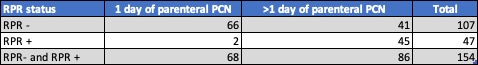
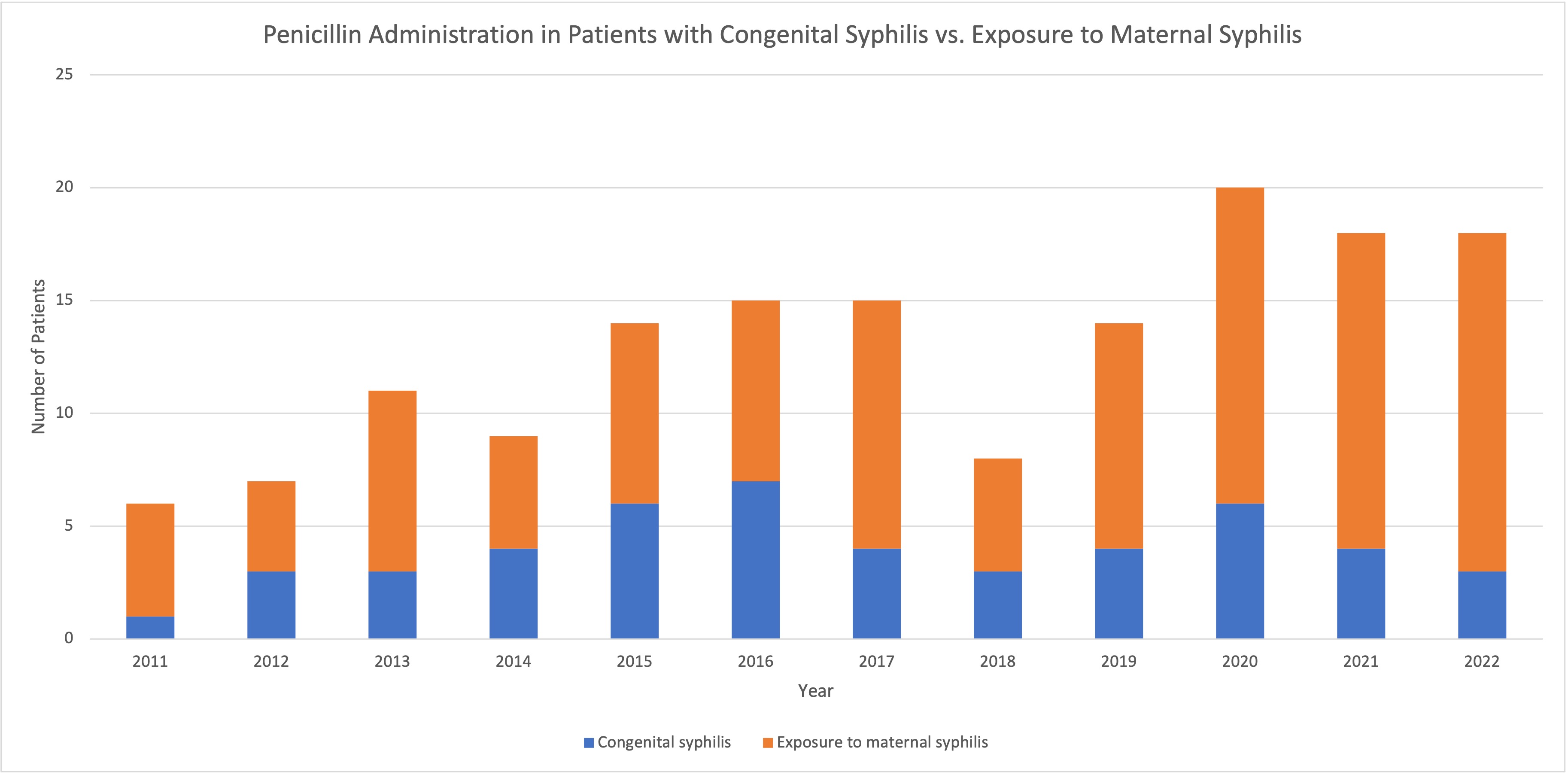
Results: 229 patients met criteria. The first cohort of 75 infants (32.8%) received penicillin for non-syphilis infections while the second 154 (67.2%) received treatment for syphilis-related indications. Within the second cohort, 31.2% of patients were diagnosed with congenital syphilis and 68.8% had varying diagnoses related to maternal syphilis exposure. Of infants who received 1 day of penicillin, 2.9% had positive RPR and of those who received >1 day of therapy, 52.3% had positive RPR. There was an overall increase in syphilis-related diagnoses in the last 11 years.
Conclusion(s): Accurate diagnosis is imperative in assessing the extent of the growing CS epidemic. Diagnostic challenges are further complicated by discordance between International Statistical Classification of Diseases (ICD) diagnosis codes and the CDC diagnostic categories. Additionally, infants with negative RPR may be diagnosed with and treated for CS but not be reported to public health departments depending on laboratory-based reporting practices. Given these discrepancies, penicillin administration may be a helpful supplementary measure of CS cases. Our review of pharmaceutical data showed an increase in CS and maternal syphilis exposure diagnoses from 2011-2022. While the latter is not equivalent to a CS diagnosis, the administration of penicillin still suggests concern for CS and should be reported as such to reduce underestimation of CS. Additionally, a standardized institutional pathway for diagnosing and reporting CS may help facilitate this process.