Medical Education
Session: Medical Education 9
511 - The impact of interprofessional simulation education in the neonatal intensive care unit: a mixed methods study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 511
Publication Number: 511.3072
Publication Number: 511.3072

Lindsay E. Gilmore, MD (she/her/hers)
Neonatal-Perinatal Fellow
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Providing excellent patient care in an intensive care unit relies on competent professionals cohesively working together. Simulation builds skills for optimal teamwork. While our institution had simulation curricula for pediatric and sub-specialty trainees, there were limited simulation opportunities for other clinical professions and no opportunities for interprofessional simulations. There was a paucity of literature studying the optimal curricula to support interprofessional simulation.
Objective: We aimed to design and implement an interprofessional simulation-based curriculum to improve clinical knowledge, teamwork, and communication skills in the Intensive Care Nursery (ICN) at the Hospital of the University of Pennsylvania (HUP).
Design/Methods: We utilized Kern’s model of curriculum development. Intended learners were nurses, respiratory therapists, advanced practice providers, pediatric residents, and Neonatal-Perinatal Medicine fellows. We conducted a needs assessment survey to assess perceived value in a simulation-based curriculum and to identify desired simulation topics. We designed scenarios to highlight identified learning gaps. We implemented the new curriculum in the ICN at HUP, conducting simulations twice a month during day and night shifts. We performed pre- and post-tests and collected evaluations of the curriculum. The tests were analyzed by comparing average score improvement. To further assess our curriculum and its impact, we conducted in-person one-on-one interviews that were analyzed using grounded theory.
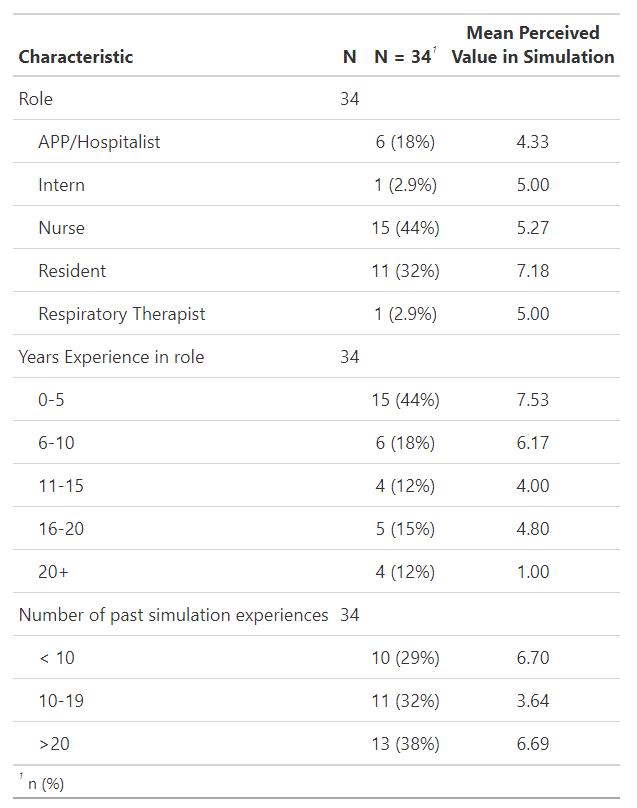
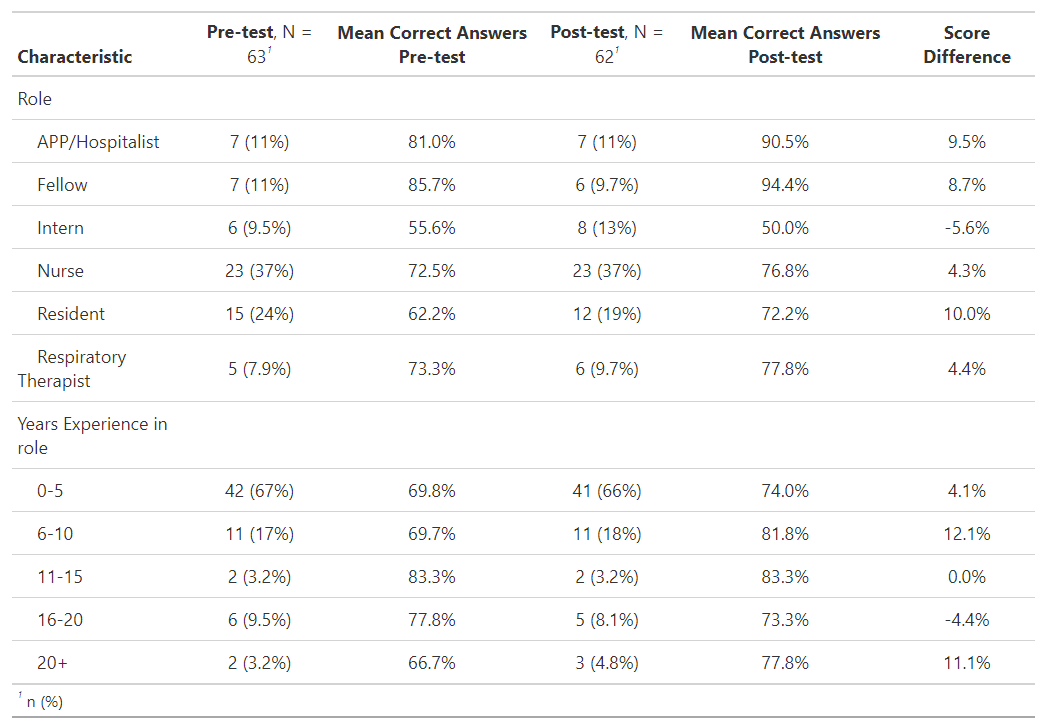
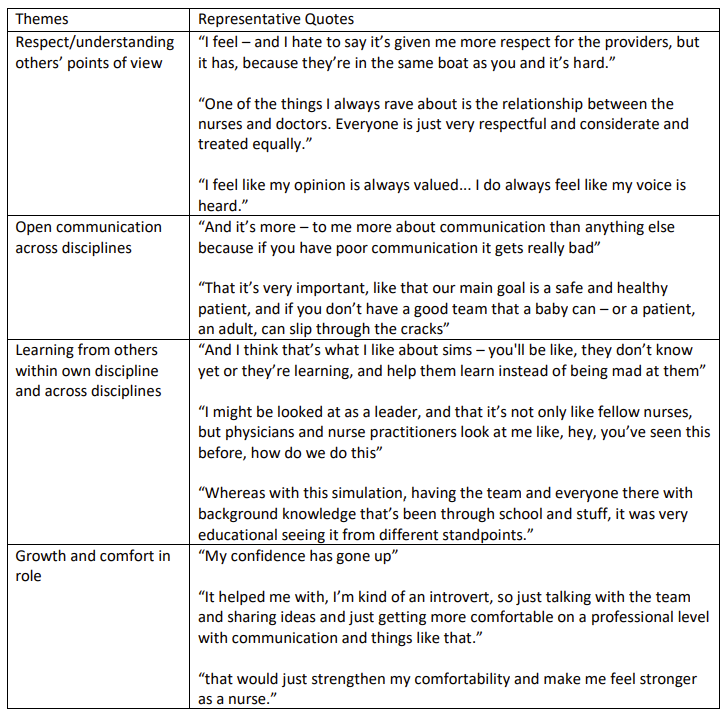
Results: The needs assessment was completed by 34 learners from all participating professions. Learners ranged in experience from 0 to 20+ years in their role and had a wide variety of prior simulation experience (Table 1). Learners identified scenarios to utilize in the curriculum with a focus on high acuity events. Average test scores improved in almost all groups of learners (Table 2). Most learners positively evaluated the simulation and debrief. Analysis of the qualitative interviews resulted in the following themes about interprofessional simulation participation: Respect/understanding others’ points of view, Open communication across disciplines, Learning from others within own discipline and across disciplines, and Growth and comfort in role (Table 3).
Conclusion(s): We successfully implemented an interprofessional simulation-based learning activity that enhanced medical knowledge, improved communication across disciplines, and contributed to growth and comfort in learners' own role. Learners found that simulation-based learning was more meaningful than anticipated.