Neonatology
Session: Neo-Perinatal Health Care Delivery 2: Epidemiology/Health Services Research
329 - Geographic variation in the racial disparity in infant mortality rates due to congenital heart disease in the United States
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 329
Publication Number: 329.1396
Publication Number: 329.1396
Julia Behrend, MD (she/her/hers)
Pediatrics Resident
Northwestern McGaw/Lurie Children's Hospital
Chicago, Illinois, United States
Presenting Author(s)
Background: African American (AA) infants are more than twice as likely to die in their first year of life than White infants. This is largely related to the elevated preterm birth rate among AA women. However, the racial disparity persists among term infants where congenital anomalies are the leading cause of death. Congenital heart disease (CHD) is the most common lethal birth defect. A prior study found a stark racial disparity in term infant mortality rates ( < 365 day, IMR) due to CHD (Collins et al, JOP, 2017). The extent to which this phenomenon varies by region of residence (Northeast, Southeast, Midwest, Southwest, and West) is incompletely understood.
Objective: To determine whether the relationship between race and IMR-CHD varies by region of residence.
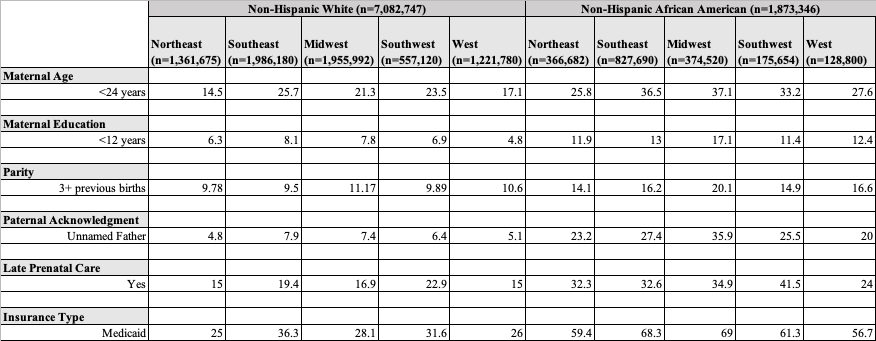
Design/Methods: Stratified and multivariable binomial regression analyses were performed on the 2016-2019 National Center for Health Statistics linked live birth-death cohort dataset of singleton, term (37-42 weeks) births to AA (N=1,873,346) and non-Hispanic White (N=7,082,747) women. Co-variates included maternal age, education, marital status, parity, prenatal care usage, pre-existing medical conditions, insurance status, and paternal acknowledgement.
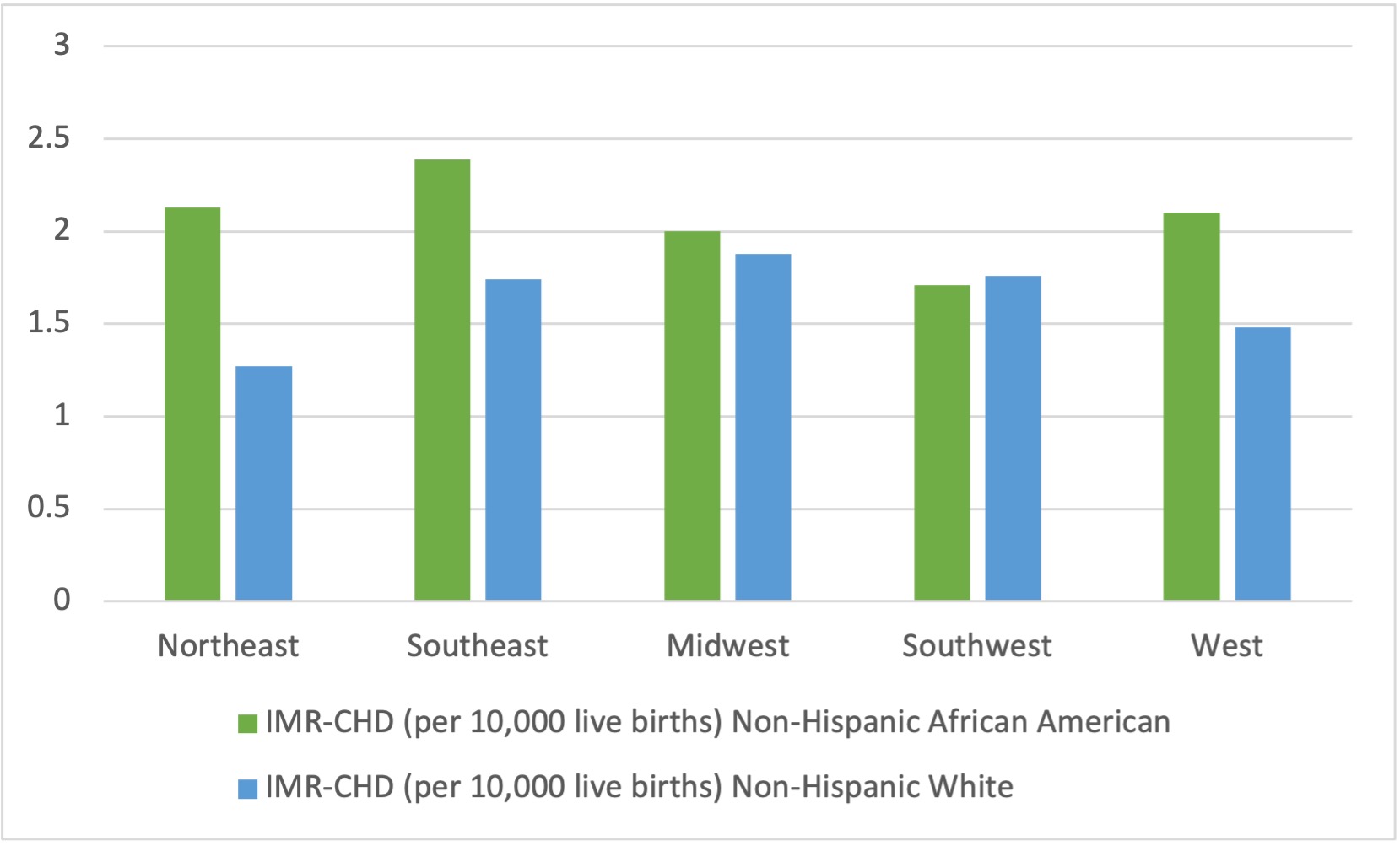
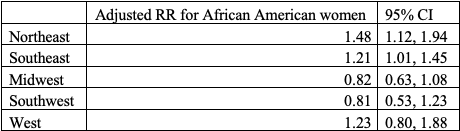
Results: The racial disparity in first-year mortality rates due to CHD was widest in the Northeast where the death rate for AA infants equaled 2.1/10,000 vs 1.3/10,000 for non-Hispanic White infants, RR (95% CI) = 1.7 (1.3, 2.2) (Figure 1). In stark contrast, both races had a similar IMR-CHD of 1.7/10,000 in the Southwest, RR equaled 1.0 (0.7, 1.5) (Figure 1). In each region, AA (compared to non-Hispanic White) infants had a greater percentage of high-risk maternal sociodemographic characteristics including low education attainment and Medicaid insurance (Table 1). Most striking, the adjusted (controlling for maternal age, education, marital status, parity, prenatal care usage, pre-existing medical conditions, insurance status, and paternal acknowledgement) RR of first-year mortality due to CHD for AA (compared to non-Hispanic White) infants ranged from 0.8 (0.5, 1.2) in the Southwest to 1.5 (1.1, 1.9) in the Northwest (Table 2).
Conclusion(s): The racial disparity in IMR-CHD is most pronounced in the Northeast and is absent in the Southwest. In the Northeast, AA race is a strong determinant of first-year mortality due to CHD independent of known traditional individual-level characteristics. These intriguing findings merit public health attention.