Medical Education
Session: Medical Education 7
441 - Insights into Graduating Residents’ Identity as Teachers: Factors Influencing Who Will Precept Medical Students in the Outpatient Setting
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 441
Publication Number: 441.1392
Publication Number: 441.1392

Helen C. Wang, MD (she/her/hers)
Associate Clinical Professor
UCSD
La Jolla, California, United States
Presenting Author(s)
Background: Primary care is the core of healthcare. Yet, teaching programs struggle to provide these experiences because of difficulty with recruitment and retention of outpatient faculty and community-based preceptors. Even with clinician-educator and primary care residency tracks, few graduating residents have the skills and desire to serve as outpatient preceptors. Understanding residents’ perspectives about outpatient precepting can better inform medical education leaders on how to inspire and prepare residents to educate trainees in the future.
Objective: Describe perspectives on outpatient precepting among graduating residents
Design/Methods: A single institution qualitative study involved 30-minute semi-structured interviews via Zoom between 4/2023-6/2023 with 13 graduating pediatric, internal medicine, or combined internal medicine/pediatric residents. Using narrative analysis, we inductively coded verbatim transcripts to generate themes and subthemes through an iterative process.
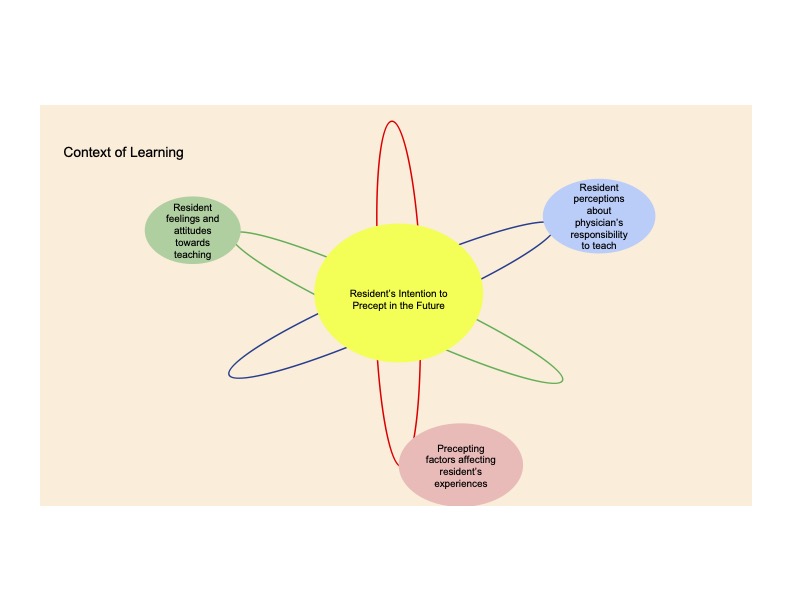
Results: Based on 105 codes, five themes were constructed regarding residents’ outpatient experiences with being precepted and being a preceptor: 1) Context of outpatient learning (eg, workplace environment, time limitations, precepting logistics), 2) Precepting factors affecting residents’ experiences (eg, preceptor attributes/style), 3) Resident feelings and attitudes towards outpatient teaching (eg, when to start precepting and for which trainees), 4) Resident perceptions about physician’s responsibility to teach (eg, viewing teaching as a moral obligation, a choice, or only for those adept at teaching) 5) Factors influencing residents’ intention to precept in the future which includes both external factors (eg, limited outpatient precepting experiences in residency) and internal factors (eg, bettering oneself or making an impact on learners). Figure 1 conceptualizes the dynamic interaction between the themes.
Conclusion(s): Robust outpatient experiences require an ample and well-prepared primary care preceptor workforce. Teaching patients, medical students, and near-peer physicians is an integral part of residency. Our study highlights the need for 1) more residency outpatient precepting opportunities 2) a pathway to re-engage residents who expressed interest in teaching, and 3) cultivation of every residents’ professional identity as a teacher. Medical education leaders must collaborate to change the culture of medical education. As medical school enrollment and residency programs increase, the responsibility to train the next generation must be borne by all physicians and not just a select few academic clinicians.