Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 1
477 - Effect of an integrated newborn care kit on neonatal and maternal health outcomes in Gilgit-Baltistan, Pakistan: Interim results of a cluster randomized controlled trial
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 477
Publication Number: 477.327
Publication Number: 477.327
- DF
Daniel S. Farrar, MPH (he/him/his)
Senior Data Analyst
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Global progress towards reducing newborn deaths is expected to fall short of the 2030 Sustainable Development Goals targets. Pakistan experiences among the highest rates of neonatal mortality (NMR) worldwide, at 42 deaths per 1000 live births. Low-cost interventions that can be delivered at-scale through community-based healthcare models are needed to prevent newborn deaths and other adverse neonatal and maternal outcomes.
Objective: We aimed to assess the effectiveness of an integrated newborn care kit (iNCK; vs. local standard of care) on neonatal mortality, when delivered by Lady Health Workers (LHWs) to pregnant women during their third trimester of pregnancy in Gilgit-Baltistan, Pakistan.
Design/Methods: We are conducting a parallel-arm, open-label, cluster randomized trial in Gilgit-Baltistan; a remote, mountainous region in northern Pakistan. Seventy-seven Union Councils (clusters) were randomized 1:1 to either the iNCK (intervention) or local standard of care (control) arm. All pregnant women in the study area were eligible to participate, and were delivered the iNCK or control by LHWs in their third trimester. The iNCK includes a clean birth kit, chlorhexidine gel, sunflower oil emollient, ThermoSpotTM temperature indicator sticker, fleece blanket, click-to-heat warmer, misoprostol tablets, and educational pictorial guide. The primary outcome is all-cause neonatal mortality, or death of a live-born newborn in the first 28 days of life. The trial launched in March 2022, and aims to enroll 27448 pregnant women by June 2024. We report interim results by blinded study arm using adjusted risk ratios (aRR) and 95% confidence intervals (CI).
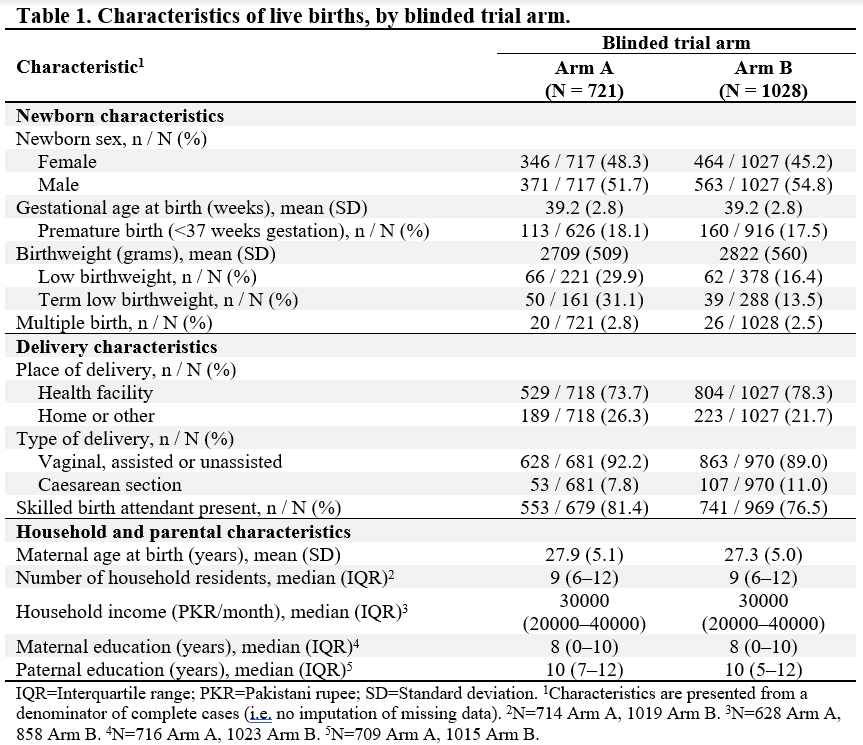
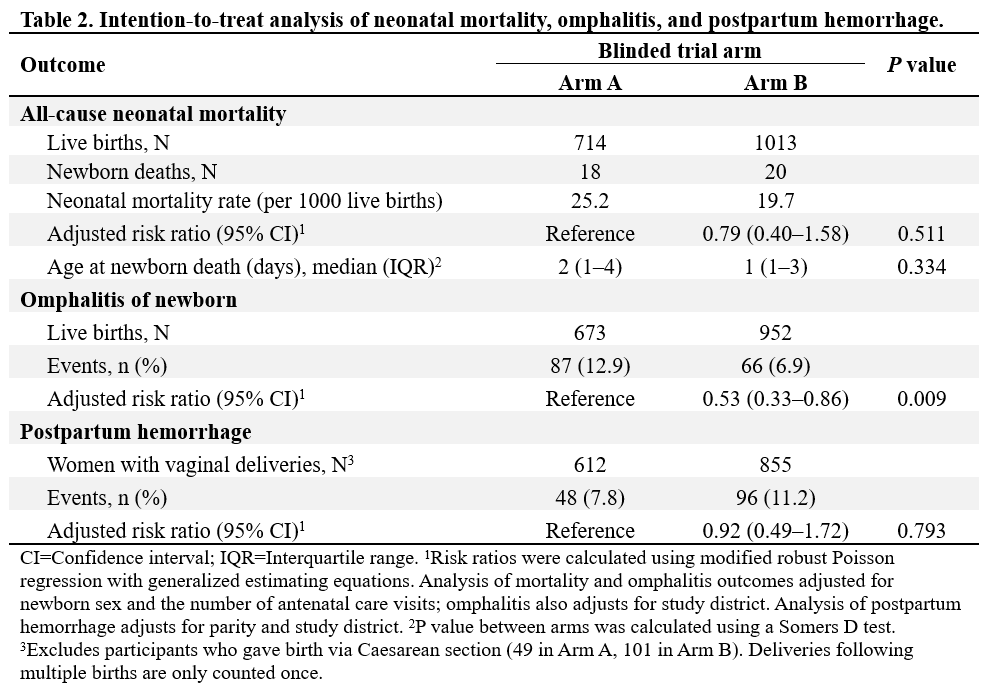
Results: As of October 2023, we have enrolled 14726 pregnant women. In interim analysis of the first 1749 live births (721 Arm A, 1028 Arm B), 47% were female and the mean gestational age at birth was 39.2 weeks (Table 1). In Arm A, 74% were delivered at a health facility versus 78% in Arm B. Eighteen newborn deaths were reported in Arm A (NMR 25.2 per 1000 live births) versus 20 in Arm B (19.7 per 1000 live births; aRR 0.79, 95% CI 0.40–1.58, p=0.51) (Table 2). The cumulative incidence of omphalitis in Arm A (13%) was significantly greater than in Arm B (7%; aRR 0.53, 95% CI 0.33–0.86, p=0.009). Among mothers who delivered vaginally, there was no significant difference in the proportion experiencing postpartum hemorrhage (aRR 0.92, 95% CI 0.49–1.72, p=0.79).
Conclusion(s): The iNCK has the potential to reduce newborn mortality and morbidity in Pakistan. Upon trial conclusion, we will generate policy-relevant evidence for Pakistan and other settings with high NMR.