Neonatology
Session: Neonatal Quality Improvement 4
69 - Simple and Effective Interventions to decrease phlebotomy losses in the Extremely low birth weight infants.
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 69
Publication Number: 69.3065
Publication Number: 69.3065
- PP
Prabhu S. Parimi, MD, MBA (he/him/his)
Division Chief, Neonatology
MetroHealth Medical Center
Cleveland, Ohio, United States
Presenting Author(s)
Background: Attention to phlebotomy losses in the neonatal ICU is key to decrease the need for packed red blood cell transfusions. Recent studies documented excessive withdrawal of blood in extremely low birth weight (ELBW) occurs due to acuity of illness, removing more blood than required for laboratory monitoring specifically during the first weeks of life. Point of care testing and in-line monitoring strategies were employed to decrease phlebotomy loss and blood transfusion in ELBW infants. Human and technological factors are important considerations to mitigate blood loss and excessive blood transfusions.
Objective: The SMART goal of this quality improvement project is to 1). Decrease the total volume of blood loss in ELBW infants during the first 7-days after birth by 10% by decreasing the number of laboratory tests, and 2). Decrease the number of blood transfusions in ELBW infants during the first 7-days after birth by10% and sustain for one year.
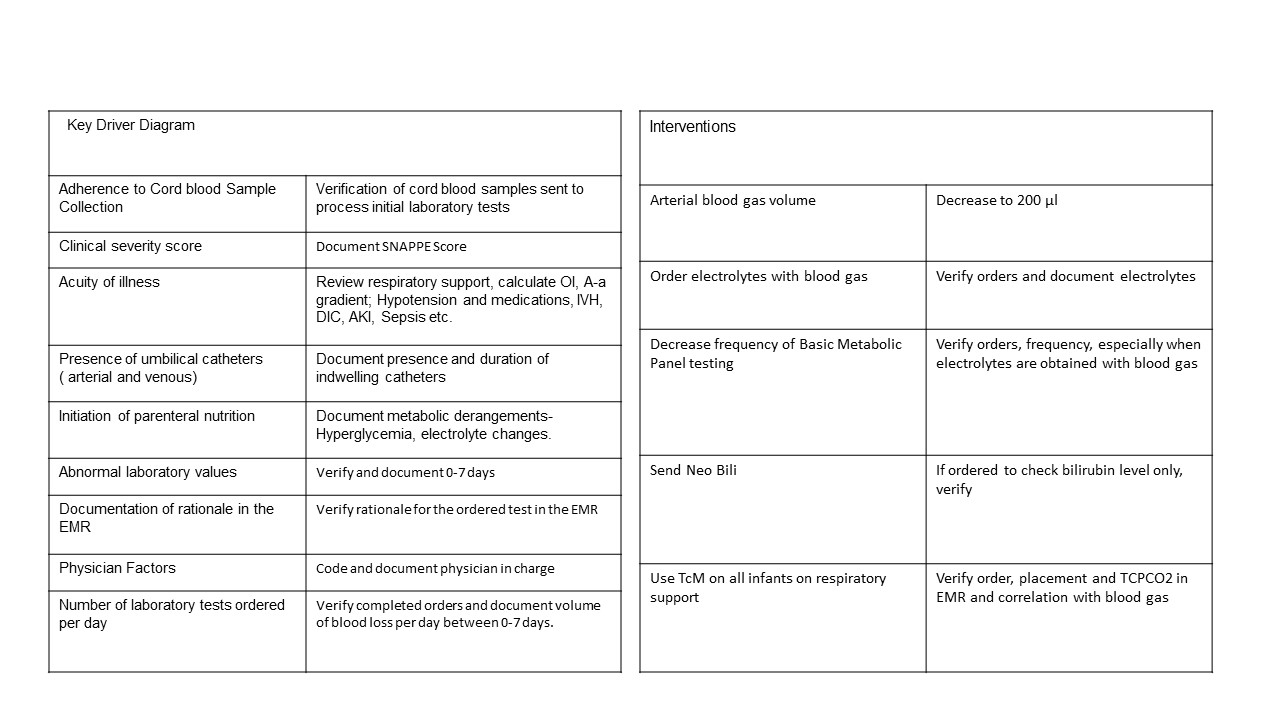
Design/Methods: As part PDSA cycle, we obtained baseline data in infants with a birth weight < 1000g. These include, number of laboratory tests ordered, cumulative blood loss and volume of PRBC transfusion during the first week. Post- baseline data, a multidisciplinary "phlebotomy loss task force" and utilized the Fishbone and outlined the key drivers (Table 1,) and decided on 1). Decreasing blood gas volume to 200 mcl; 2). Order electrolytes with blood gas; 3). define indications to obtain basic metabolic panel; 4). Order neo bilirubin to measure bilirubin level; and 5). Utilize TcCO2 monitoring to trend CO2 to decrease frequency of blood gases.
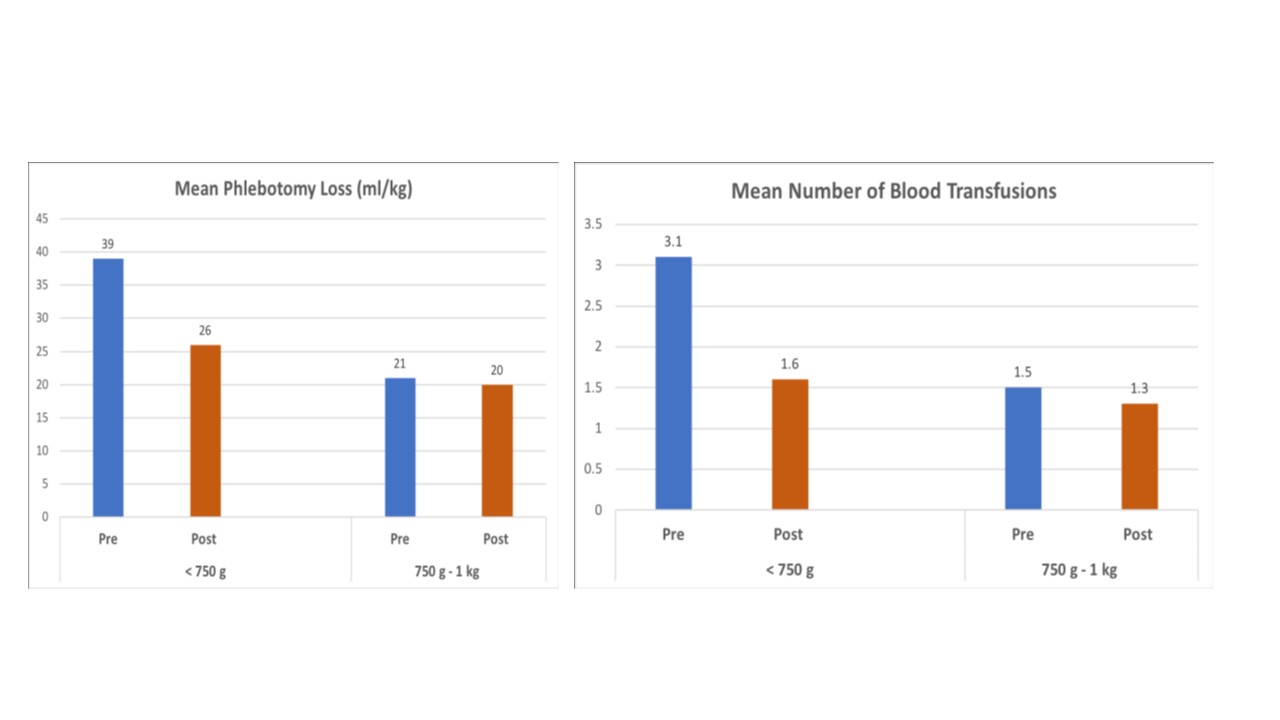
Results: Using the Mann-Whitney U test, the results showed that the median phlebotomy loss per infant decreased from 27 ml/kg to 22 ml/kg post-intervention. There was a significant reduction of 18.5% (p= 0.005). The median number of blood transfusions significantly decreased by 33.3% in the group of infants with a BW of less than 750 g (p 0.034).
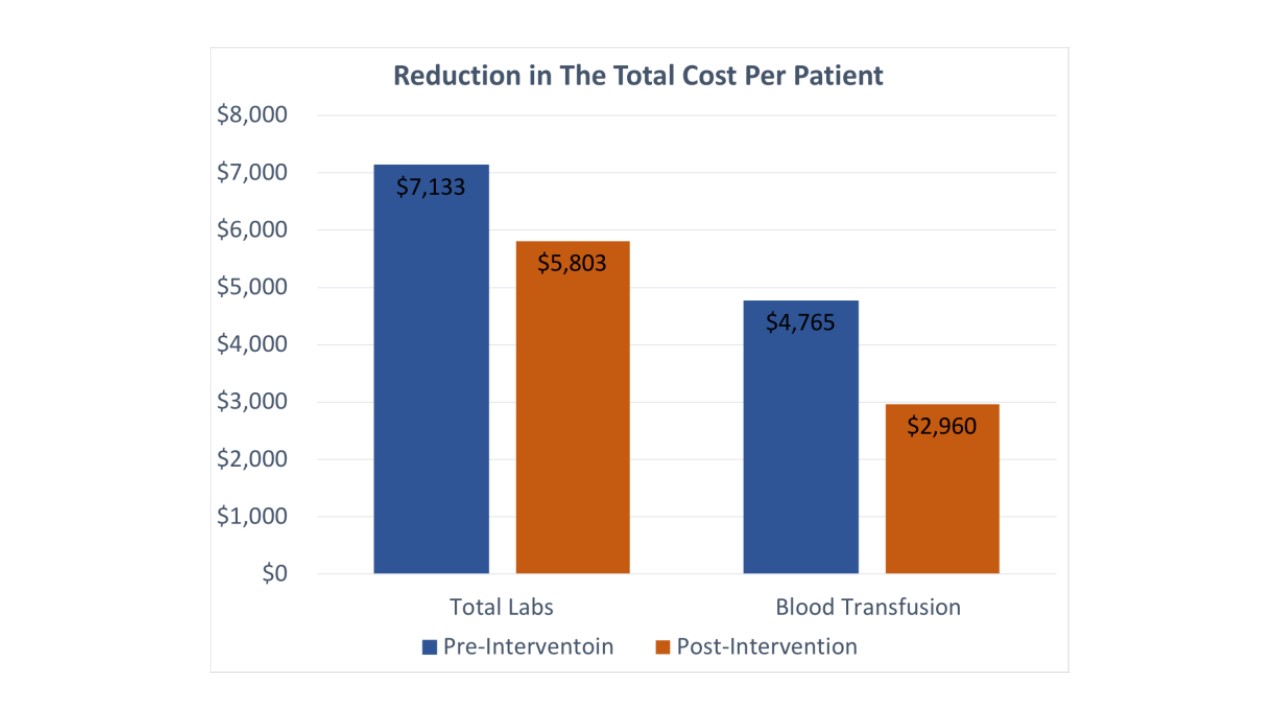
In the pre-intervention group, the total cost to process laboratory specimens and administer blood transfusion per patient was $ 7135 and $ 4765, respectively. Post-intervention, the associated costs decreased to $ 5803 and $ 2960, respectively, indicating a per-patient reduction of 18.7% and 37.9%. (Figure)
Conclusion(s): Implementation of simple intervention strategies led to significant reduction in phlebotomy loss, blood transfusions and laboratory and blood transfusion associated costs.