Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 4
258 - Inequities in Hospital Admissions for Growth Faltering
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 258
Publication Number: 258.1376
Publication Number: 258.1376

Katherine Salada, MD (she/her/hers)
Assistant Professor
University of Michigan Mott Children's Hospital
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Growth faltering (GF), previously Failure to Thrive, is defined as weight for length or body mass index (BMI) less than the 5th percentile or when weight negatively crosses >2 major percentile lines. GF is typically due to a complex relationship of medical, developmental, nutrition, and psychosocial factors resulting in malnutrition. Literature is lacking regarding whether inequities exist in the treatment of patients with growth faltering by factors such as race and ethnicity.
Objective: Describe potential inequities due to race and ethnicity in admission criteria and inpatient treatment for children with a diagnosis of GF.
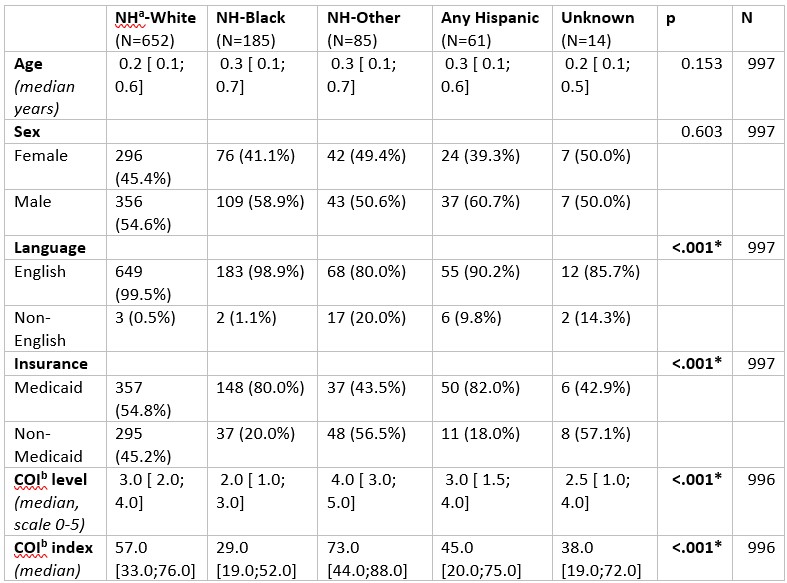
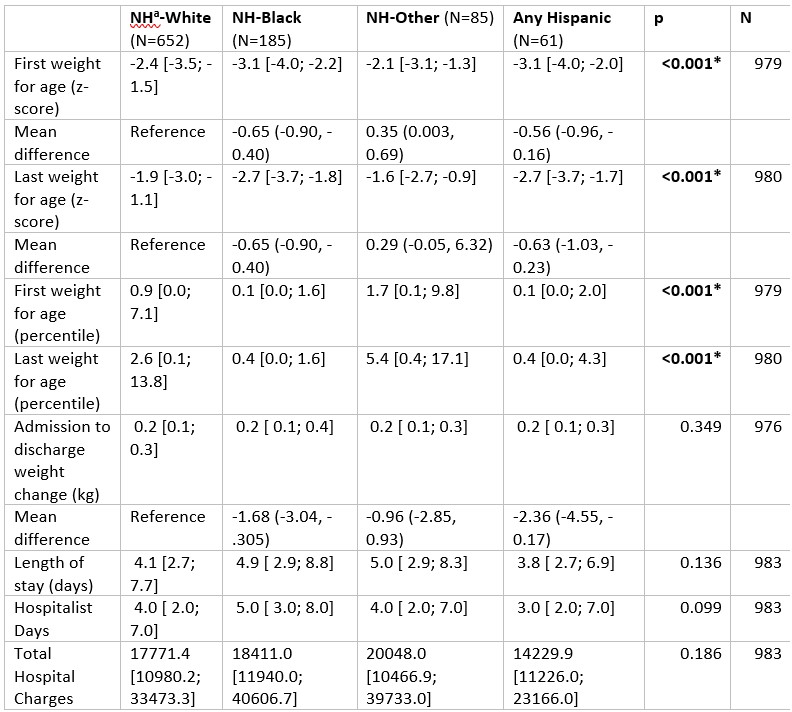
Design/Methods: A retrospective chart review was conducted to identify all children 1 to 24 months of age admitted to a large tertiary children’s hospital with a primary or admission ICD9 or ICD10 diagnosis of GF (or synonymous term) from January 2012 through January 2022. Demographic data, growth parameters at admission/discharge, and inpatient treatment course (labs, consults, interventions) were obtained from the electronic medical record. Data was analyzed via generalized linear models using identity link for continuous outcomes and logit link for binary outcomes.
Results: The study population (n=997) was predominately Non-Hispanic (NH)-White (65%), male (55%), and were Medicaid recipients (60%) (Table 1). NH-Black patients had the lowest child opportunity index level score (2.0, SD 1; 3.0) of the cohort (p < 0.001), suggesting lower socioeconomic status. NH-Black patients and Hispanic patients had lower admission weight for age z-scores (-3.1) compared to NH-White patients (-2.4; p=0.00). There was no difference in median change in weight during admission or total length of stay by race/ethnicity. NH-Black patients and Hispanic patients had lower discharge weight for age z-scores (-2.7) compared to NH-White patients (-1.9; p< 0.001). During admission, NH-Black patients were the most likely group to receive social work (46%, p=0.02) and dietician consults (83%, p=0.02). However, NH-White patients had higher rates of lactation consults (26%) compared to NH-Black (14%) and Hispanic (12%) patients (p < 0.001). Other consulting service rates, labs, and imaging did not vary by race/ethnicity.
Conclusion(s): Our study notes difference in admission/discharge growth metrics and consult services obtained based on race and ethnicity for children admitted for GF. Further study is needed to understand what factors contribute to these inequities and to implement targeted system changes to help mitigate, or better yet eliminate, these inequities.
.jpg)
