Critical Care
Session: Critical Care 2
127 - Importance of Breathing When It Is Busy: A Novel PICU Activity Score Related to Asthma Medication Delay
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 127
Publication Number: 127.3046
Publication Number: 127.3046
- MF
Michael L. Forbes, MD
Chief Academic Officer & Professor of Pediatrics
Akron Children's Hospital | Northeast Ohio Medical University College of Medicine
Akron, Ohio, United States
Presenting Author(s)
Background: Seasonal variation in PICU volume and acuity can create staffing mismatches that result in care delay, care failure, and patient harm. While provider staffing tends to be fixed, critical care nursing staffing models vary, are often based on the average daily census and fail to account for this natural variation. There is a need to develop meaningful metrics that incorporate the natural volume-acuity variation that can be used to inform dynamic, data-informed staffing models.
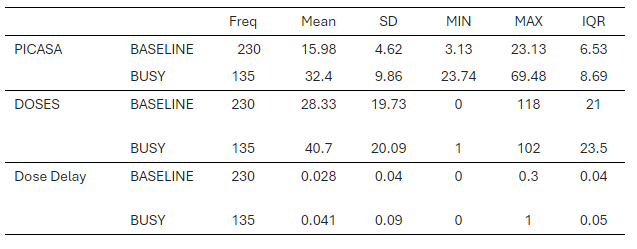
Objective: We hypothesized the PICASA score would identify increased asthma care delay with increased PICU activity. Usual descriptive statistics were calculated, and the Mann-Whitney test compared care delay rates between baseline and busy days. Significance is reported as p< 0.05, and data are presented as Baseline vs BUSY unless otherwise stated.
Design/Methods: Based on work by Pagel, et al, the study PICU (23-bed), using the local VPS database, developed the Pediatric Intensive Care Activity Score-Akron (PICASA), an activity score based on total daily encounters, percent occupancy, the insertion or presence of critical care devices (endotracheal tubes, ECMO cannulation, etc), as well as critical procedures (CPR, etc). The Bollinger bands methodology was then applied to derive the 95% confidence interval for the daily score. PICASA scores above the 70th and 90th percentiles were defined as “BUSY”. The PICU has had a standardized critical care asthma pathway where medication administration delay was defined as >30 minutes after prescribed. Scheduled aerosolized albuterol given in calendar year 2015 was used in this pilot as the number of scheduled treatment events was greater than either methylprednisolone or ipratropium.
Results: There were 12,010 doses of albuterol scheduled during the pilot study. Total daily doses ranged from 0 – 118. The overall PICASA score was 22.05 + 10.60, and average daily doses were 32.9+20.72, underscoring the seasonal variation. The table is a summary of BASELINE vs BUSY values. There was a higher rate of care delay on busy days (n=135) than baseline (n=230), (4.1 + 0.09% vs 2.8 + 0.04%, p=0.03).
Conclusion(s): The heuristically derived PICASA score appears to identify single medication administration care delay when activity exceeded the 70th percentile for this PICU. The pilot satisfies face, construct, and criterion validity and warrants further investigation. The value of a locally derived metric of PICU activity may signal increased likelihood of care delay would be an asset in our quality improvement armamentarium. Additional modeling using all scheduled PICU medications from 2015–2022 is underway.