Neonatology
Session: Neonatal Infectious Diseases/Immunology 3
623 - Frequency of Hepatitis C Screening Among Women with Substance Abuse Disorder (SUD) Who Deliver at a Single Regional Newborn Center
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 623
Publication Number: 623.357
Publication Number: 623.357
- DR
Divya Rana, MD
Associate Professor
University of Tennessee Health Science Center College of Medicine
University of Tennessee Health Science Center
Memphis, Tennessee, United States
Presenting Author(s)
Background: An increase in Hepatitis C infection (HepC) has been reported among US adults with opioid use disorder (OUD). Given the current increase in the risk of hepatitis C infection, routine screening is recommended for all pregnant women, however, many centers are still practicing “risk-based” screening. With current levels of opioid use, especially with rising fentanyl abuse universal screening for HepC should be done. Neonatal outcomes of infants born to mothers with newly diagnosed active hepatitis C infection and substance use disorder (SUD) including opioid use disorder (OUD) and are unknown
Objective: To assess frequency of HepC screening of mothers of infants born at a large newborn center in Memphis, TN.
Design/Methods: This is a prospective cohort study of neonates born to mothers with evidence of prenatal use of prescribed or non-prescribed substances from January 2018 to December 2022. Maternal substance use was confirmed with self-report as well as a positive urine toxicology and an umbilical cord (UCT) testing. Infant and maternal demographics were recorded. Hepatitis C RNA quantitative and log(10) results were recorded.
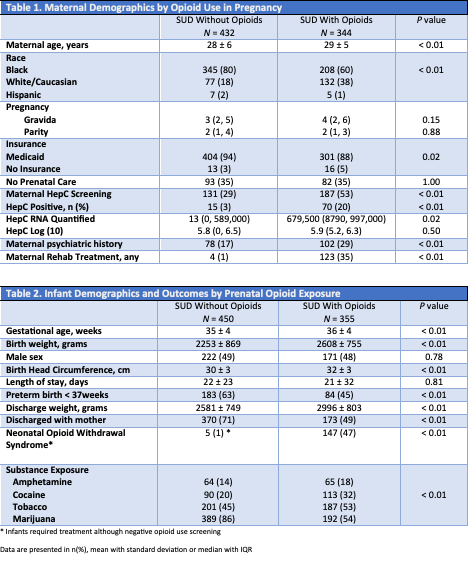
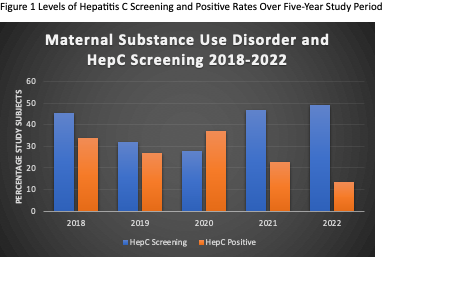
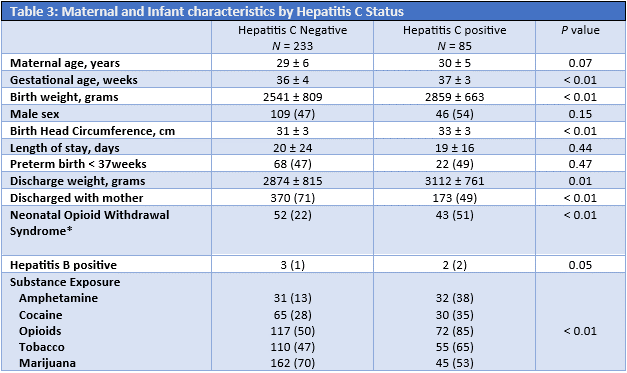
Results: A total of 776 and their 805 infants were enrolled, of these 44% (355/805) infants had opioid exposure. Average maternal age of 29 ± 6 years, gestational age of 35 ± 3 weeks, birthweight of 2410 ± 839 grams. Overall, during pregnancy only 41% (318/776) mothers had a HepC screening completed. Maternal, neonatal demographics and outcome are shown in tables 1&2. Of note, 37% (70/187) mothers with OUD screened positive for HepC versus only 11% (15/131) for non-opioid SUD mothers. Among all 85 mothers with positive Hepatitis C, a reported hepatitis C quantitative RNA level, 1,130,869 ± 1,996,280 copies, and HepC Log (10) 4.93±2.3 was reported. Table 3 summarizes group characteristics based on HepC positive status. Mothers were more likely to be screened for Hepatitis C with Heroin abuse OR 3.2 (CI95% 1.90, 5.49) and if they were enrolled in opioid treatment program OR 2.5 (CI95% 1.53, 3.92). Compared to non-opioid group the Hepatitis C RNA Quantified levels among opioid using mothers were much higher, p 0.02. None of the infants had HepC testing done during initial hospitalization.
Conclusion(s): Hepatitis C screening among women with substance use disorder is low, inconsistent and remains under-reported. Despite current recommendations, Hepatitis C screening was more commonly performed in women with heroin use or if enrolled in opioid program. Mothers with opioid use during pregnancy may have very high levels of hepatitis C RNA increasing perinatal transmission risk.