Emergency Medicine
Session: Emergency Medicine 10: Trauma
397 - External Validation of the Surgical Intervention for Traumatic Injuries (SITI) score in children
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 397
Publication Number: 397.3029
Publication Number: 397.3029

Bergthor Jonsson, MD (he/him/his)
Pediatric Emergency Medicine Fellow
Children's Hospitals and Clinics of Minnesota
Woodbury, Minnesota, United States
Presenting Author(s)
Background: The Surgical Intervention for Traumatic Injuries (SITI) score is a clinical score intended to predict the likelihood of a patient with traumatic brain injury (TBI) needing surgical decompression and to improve communication between providers. The score ranges from 0 to 11 and incorporates findings on clinical examination, such as Glasgow coma scale (GCS) and unilateral dilated pupil, and neuroimaging (midline shift, temporal lobe pathology and epidural hematoma).
Objective: The aim of the study was to examine the performance of the SITI score to predict the need for surgical decompression in pediatric patients with TBI and to identify the optimal threshold for a positive score.
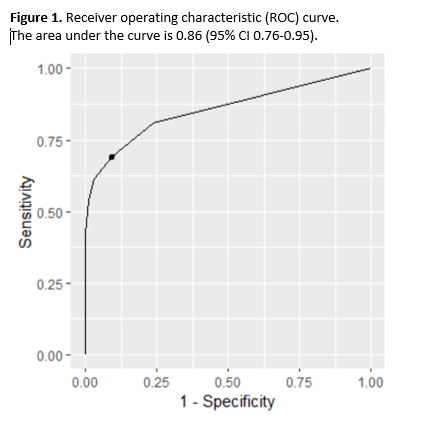
Design/Methods: This was a single center retrospective chart review study of pediatric patients ( < 18 years of age) diagnosed with TBI as determined by International Classification of Disease (ICD) codes, between June 1, 2003 and May 31, 2018. Patients with penetrating injuries were excluded. Data was abstracted from the electronic medical records by research assistants and all cases were scored by a physician who was blinded to the outcome. Continuous variables were compared using Wilcoxon rank sum test. Categorical variables were compared using chi-square test or Fisher exact test. We created a dichotomous variable indicative of patients SITI scores meeting or not meeting the threshold. Specificities, sensitivities, positive predictive values, and negative predictive values were calculated for different SITI score cutoffs to identify the optimal cutoff for a positive score. Receiver operating characteristic (ROC) curve was created to evaluate the score performance.
Results: There were 633 encounters with TBI, of which 26 (4.1 %) underwent surgical decompression (Table 1). The mean SITI score for the operative group was 4.08 and 0.37 for the non-operative group. In the operative group 17 (63%) had a score of ≥2 compared to 53 (9%) in the non-operative group (P < 0.01). All components of the SITI score were more often present in the operative group (Table 2). SITI score had acceptable discrimination for predicting surgical decompression (area under the curve 0.86; 95% CI 0.76-0.95; Figure 1). Using a score of 2 or greater as cutoff for a positive score the sensitivity was 0.69, specificity of 0.91, positive predictive value of 0.25 and negative predictive value of 0.99.
Conclusion(s): A SITI score of 2 or greater identifies children with TBI who may need surgical decompression with moderate sensitivity and high specificity. The lower sensitivity compared to prior studies may limit the utility in clinical practice.
.png)
.png)
