Neonatology
Session: Neonatal Nephrology/AKI 1
43 - Racial Disparities in In-Hospital Mortality and Acute Kidney Injury in Infants Admitted to the Neonatal Intensive Care Unit
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 43
Publication Number: 43.1994
Publication Number: 43.1994

Jennifer Rumpel, MD
Neonatologist
University of Arkansas for Medical Sciences College of Medicine
Little Rock, Arkansas, United States
Presenting Author(s)
Background: ADVANCE is an epidemiologic investigation of acute kidney injury (AKI) in level IV neonatal intensive care units (NICUs) in the United States that participate in the Children’s Hospitals Neonatal Consortium (CHNC).
Objective: This analysis focuses on differences in AKI and in-hospital mortality by infants’ maternal race. Previous epidemiologic literature, has not investigated differences with mortality and AKI prevalence by maternal race in the critically ill level IV NICU population.
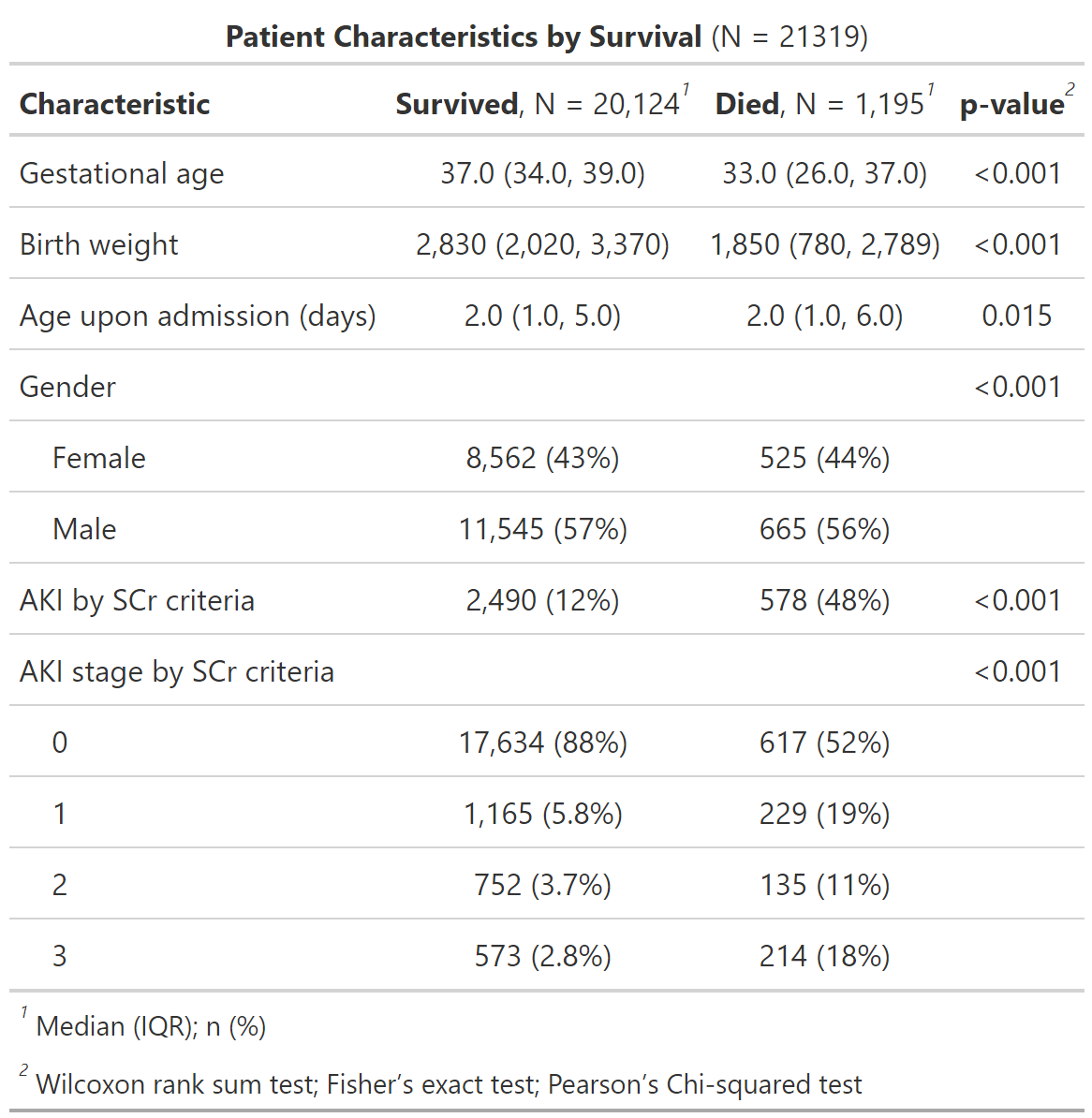
Design/Methods: The analysis included infants admitted to eight centers from 2011-2023. Demographic and mortality data from the CHNC Database were linked to electronic health record data obtained by standardized biomedical informatics scripts at each center. Infants >30 days upon admission were excluded. AKI was defined using neonatal modified Kidney Disease: Improving Global Outcomes serum creatinine-only criteria. All serum creatinine values from each participant’s entire hospitalization were extracted. A logistic regression model for mortality was built with the exposure of maternal race and covariates of AKI, birth weight, gestational age, and site. An additional logistic regression model was built for AKI with maternal race as the exposure and covariates of birthweight, gestational age and site.
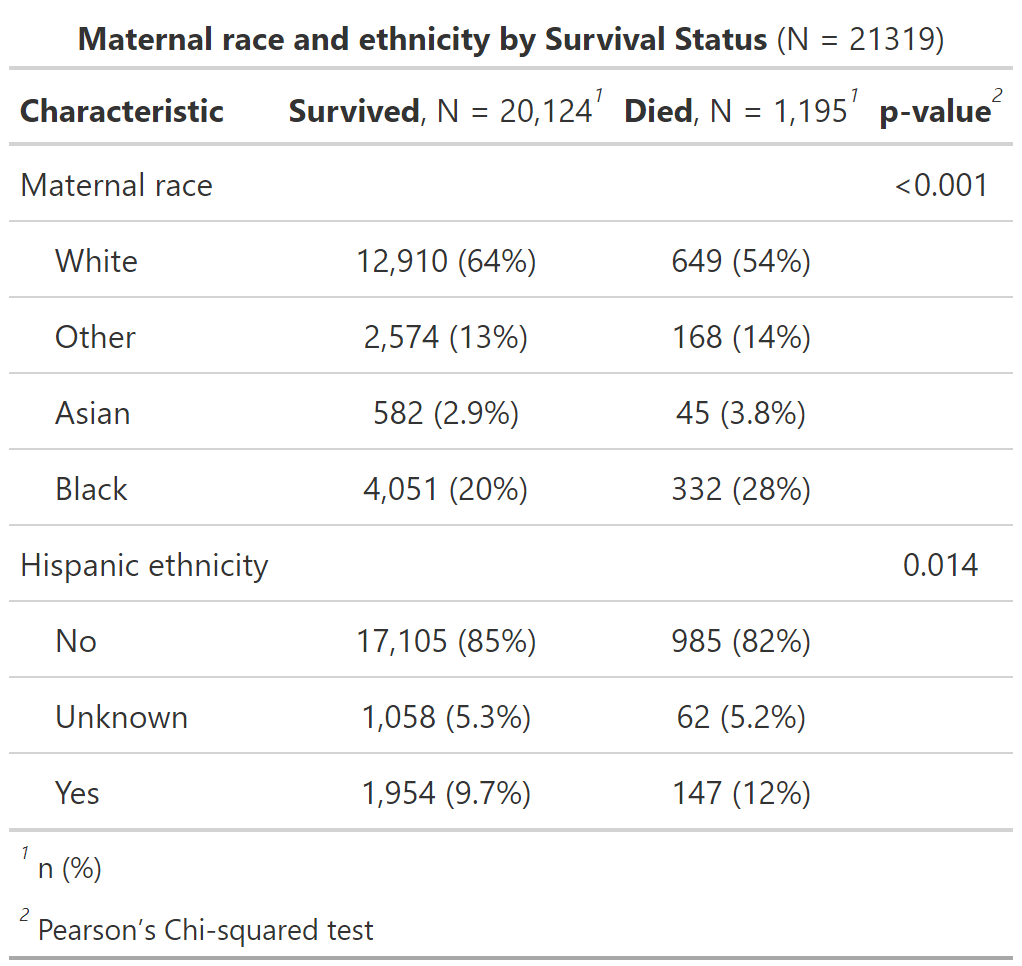
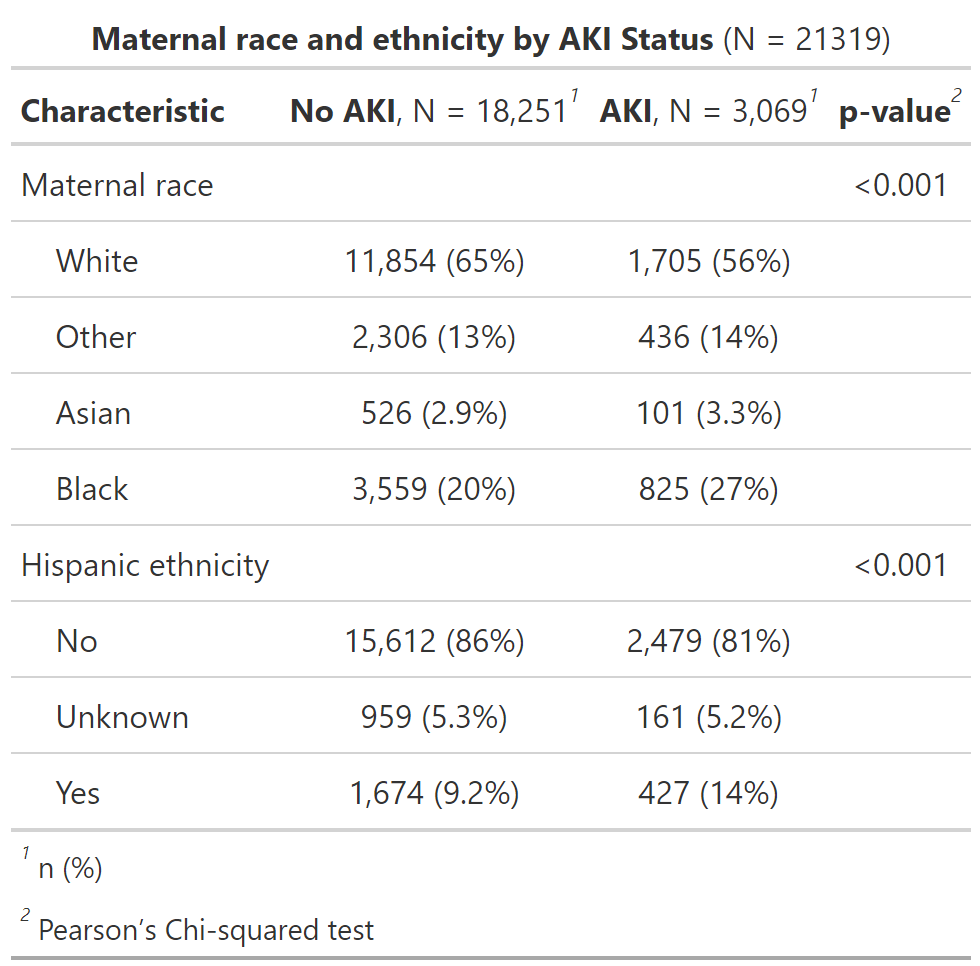
Results: AKI prevalence was 14% in this cohort of 21,219 infants. Infants with White mothers had the lowest AKI prevalence while infants born to Black mothers had the highest AKI prevalence (13 vs. 19%, p= < 0.001). When compared to infants born to White mothers, neonates born to Other and Black mothers had a 23-24% higher adjusted odds of AKI (Other: OR 1.23 95%CI 1.07-1.41; Black: OR 1.24 95%CI 1.12-1.37). Mortality for the overall cohort was 5.6%. Infants with White mothers had the lowest mortality at 4.8%, and infants born to Black mothers had the highest mortality at 7.6% (p < 0.001 ). Other and Asian maternal race were associated with higher adjusted odds of mortality of 46-47% (Other: OR 1.46 95%CI 1.18-1.81; Asian: OR 1.47 95%CI 1.03-2.05), and Black maternal race was associated with higher adjusted odds of mortality by 22% (OR 1.22 95% CI1.05-1.42), when compared to White mothers.
Conclusion(s): We report significant differences in in-hospital mortality and AKI prevalence by maternal race. Future investigation will focus on including additional socioeconomic variables, perinatal characteristics and comorbidities into the models of mortality and AKI. The goals of this work are to reduce inequities and improve outcomes through the reduction of in-hospital mortality and the morbidities associated with AKI.