Nephrology
Session: Nephrology 4
18 - Associations between Caregiver Anxiety and Childhood Blood Pressure and Adiposity
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 18
Publication Number: 18.1999
Publication Number: 18.1999
- ZP
Zahra Pirani, MD (she/her/hers)
Resident Physician
Cohen Children's Medical Center
Queens, New York, United States
Presenting Author(s)
Background: Environmental and socioeconomic stressors early in life are known to be associated with dysregulation of the body’s stress system, cortisol levels, and immune function, leading to the development of hypertension, obesity, and diabetes. Familial mental health is also associated with these stressors and can affect the development of metabolic syndrome in children. However, there are few studies specifically exploring cross-sectional associations between caregiver anxiety and abnormalities in pediatric blood pressure and BMI.
Objective: To assess the cross-sectional associations between self-reported caregiver anxiety and children’s systolic and diastolic blood pressure indices and BMI z-score.
Design/Methods: Between December 2022 and May 2023, caregivers attending their child’s well visits at a large urban primary care practice in New York were screened for anxiety using the 8-item NIH PROMIS-Anxiety Short Form (NPASH), assessing symptoms in the last 7 days. A retrospective chart review of their children (ages 2-17) was conducted to collect casual BP and height/weight measured at the visit. BP was indexed to the 95th%ile. Hypertensive BP status was classified based on casual BP ≥95th%ile for children < 13 years or ≥130/80 mmHg for children ≥13 years. BMI z-scores were calculated and obesity was defined as BMI z-score ≥2. Linear and logistic regression analyses examined the associations between caregivers’ NPASH scores and (1) children's BP (SBPi, DBPi, hypertensive BP status) adjusted for age, sex, and BMI z-score and (2) children’s adiposity (BMI z-score, obesity) adjusted for age and sex.
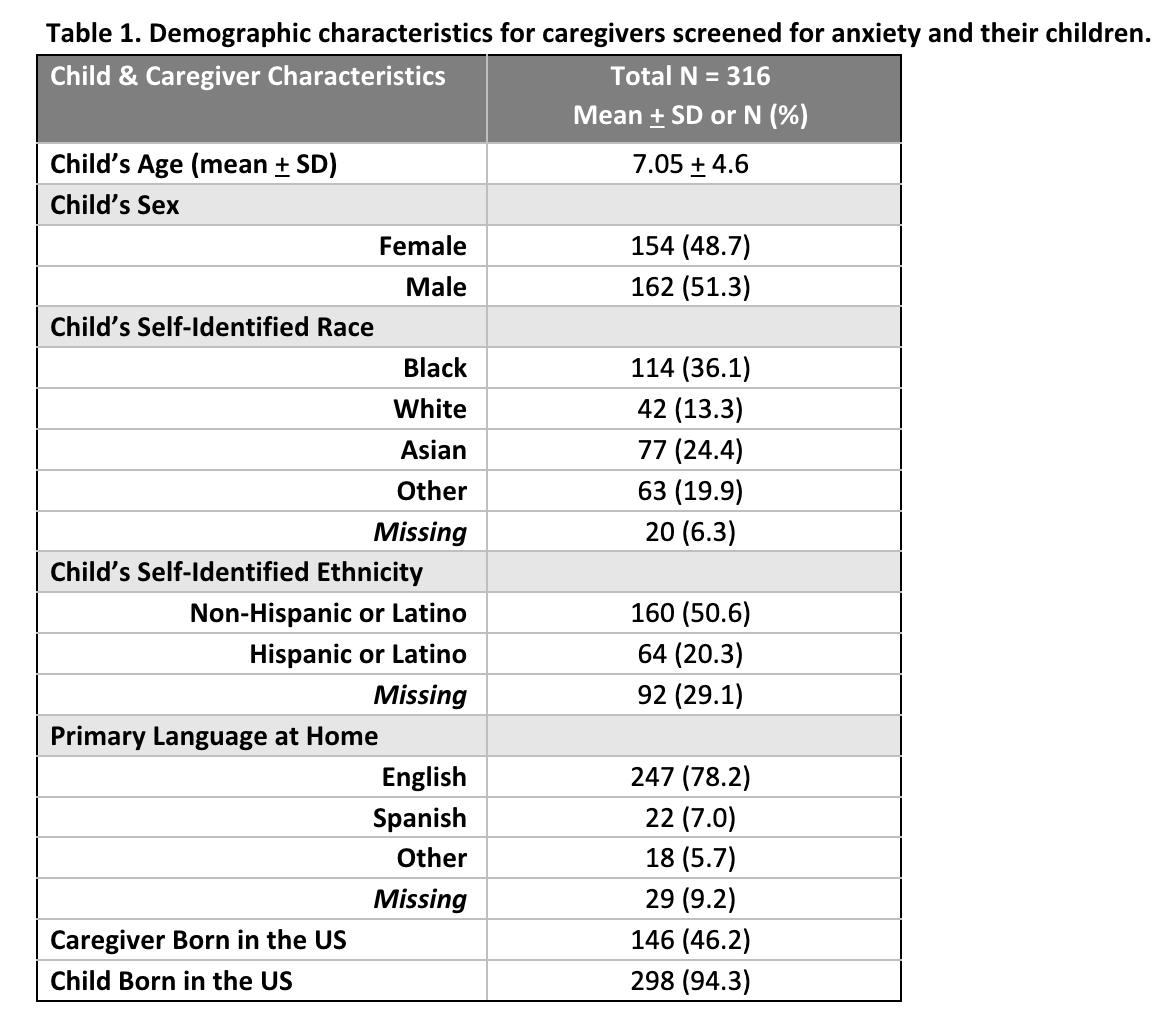
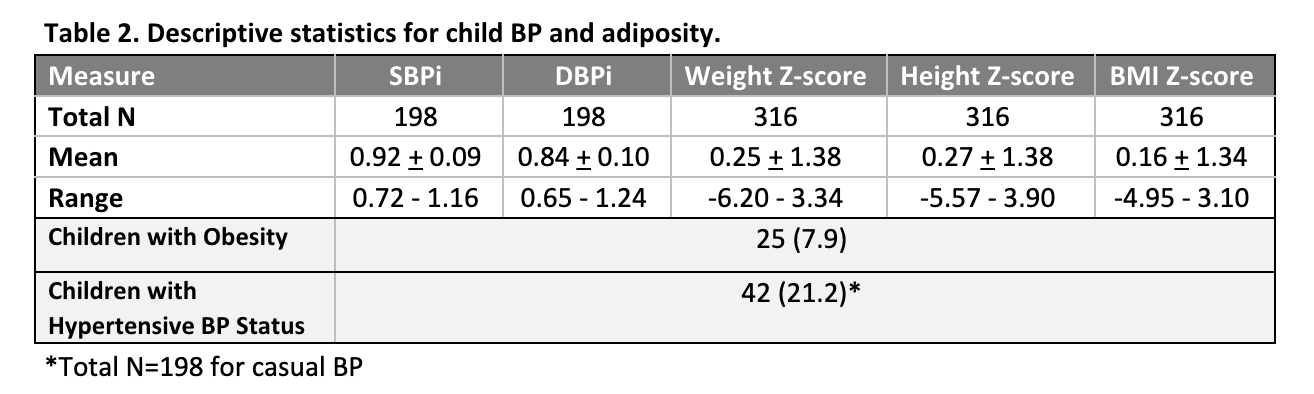
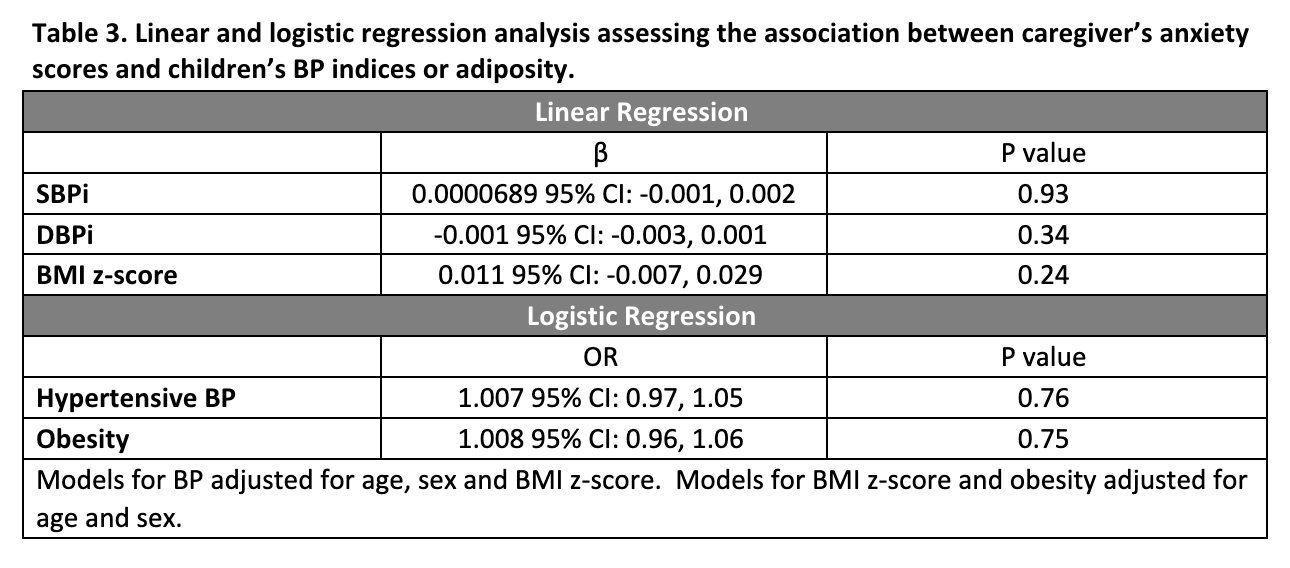
Results: The sample population was predominantly English-speaking and non-white with mean age 7.05 years (SD 4.6) (Table 1). 316 caregivers completed the NPASH. The mean T-score was 41.5 (SD 8.0, range 37.1 to 69.8), indicating average anxiety similar to the general population. For their children, mean BMI z-score was 0.16 (SD 1.34, range -4.95 to 3.10). BP was measured for 198 children, with mean SBPi 0.92 (SD 0.09, range 0.72 to 1.16) and DBPi 0.84 (SD 0.10, range 0.65 to 1.24) (Table 2). In adjusted regression analyses, there were no significant associations between caregiver’s NPASH score and child’s BP or adiposity (Table 3).
Conclusion(s): Among this diverse participant population, there was no significant cross-sectional association between caregiver’s anxiety scores and children’s BP indices or adiposity. These findings suggest that longitudinal accumulation, rather than short-term instances, of familial mental health stressors may be more influential in the development of hypertension or obesity in children.