Critical Care
Session: Critical Care 1
113 - Protocolized Sedation Eliminates Disparities in Post-Operative Pain Control
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 113
Publication Number: 113.3004
Publication Number: 113.3004
.jpg)
Nikki Lawson, MD (she/her/hers)
Pediatric Critical Care Fellow
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Disparities in congenital heart disease are associated with higher illness severity, complication rates, and mortality in non-white and publicly insured patients. Non-white patients also demonstrate worse pain control in acute care settings than white patients with similar complaints.
Objective: This study aims to describe differences in sedation and analgesia in pediatric patients undergoing cardiac surgery according to patient race, ethnicity, and language.
Design/Methods: This is a single-center, retrospective, observational cohort of index cardiac surgeries of children admitted to the cardiac intensive care unit from 7/1/2018 to 6/30/2022. Patients were excluded if > 18 years, or had a pre-existing tracheostomy, chronic renal replacement therapy, non-cardiac surgery in the same admission, or required mechanical circulatory support. Exposure variables include patient race, ethnicity, language, age, gender, postoperative mechanical ventilation, and delayed sternal closure (DSC). Primary outcomes are weight-adjusted morphine equivalent dose of opioids, midazolam equivalent dose of benzodiazepines, and of dexmedetomidine in the first 72 postoperative hours. Patient characteristics and outcomes were summarized using mean with standard deviation, median with 25th and 75th percentiles, and frequency with percentage. Wilcoxon rank sum test, Chi-square test, and Fisher's exact test were used to compare characteristics and outcomes. Multivariable quantile regression was performed.
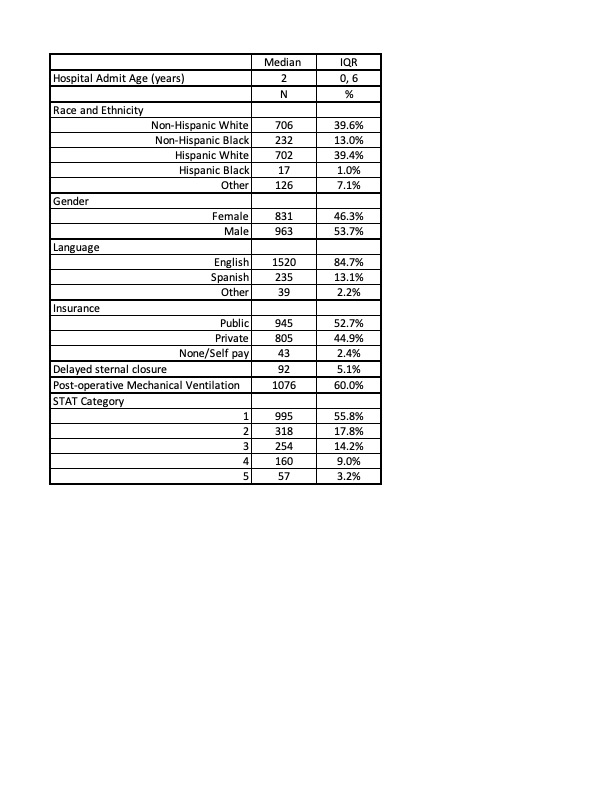
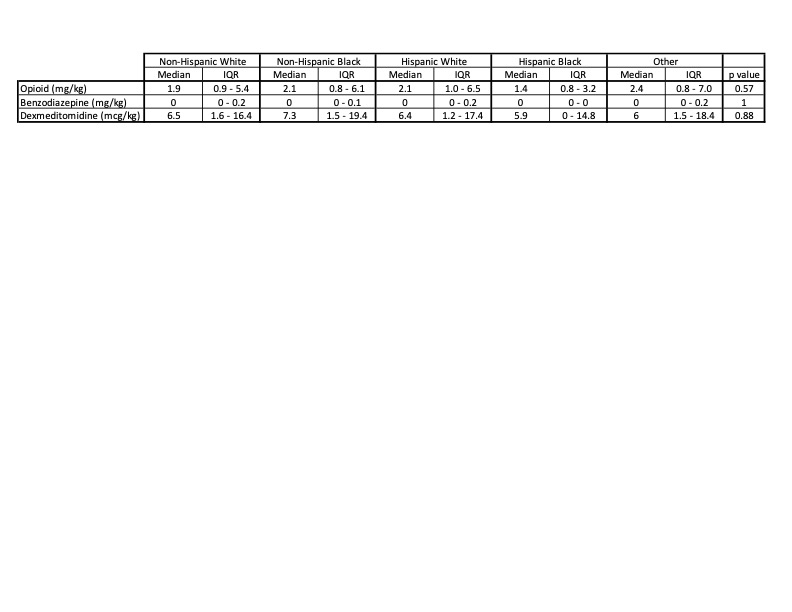
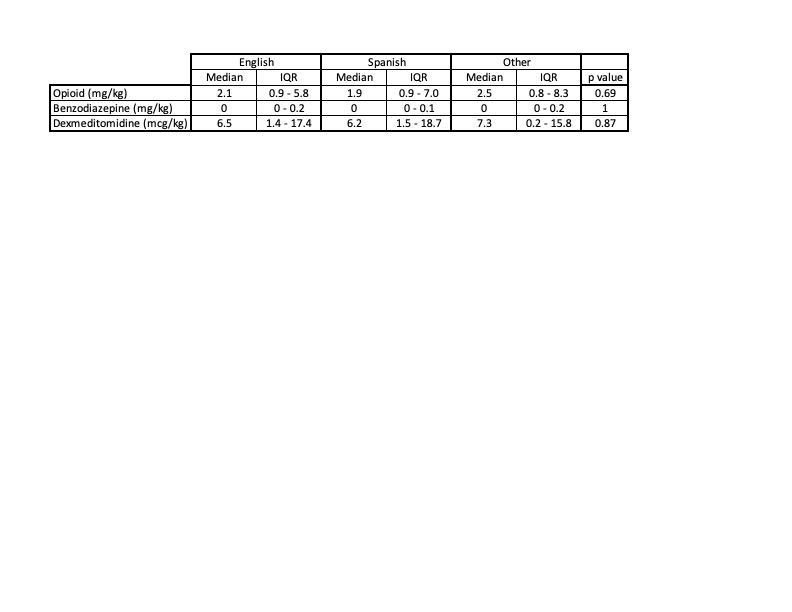
Results: There were 1794 postoperative admissions with demographics displayed in Table 1. 100% of patients received opioids, 42.5% benzodiazepines, and 85% dexmedetomidine. There were no differences in opioid, benzodiazepine, or dexmedetomidine doses according to patient race, ethnicity, or preferred language (Table 2 and 3). Regression analysis for opioids and benzodiazepines demonstrates patients with DSC, longer length of stay and mechanical ventilation received higher doses, but race, ethnicity, and language were not associated with difference in dose. Multivariable regression for dexmedetomidine demonstrated similar results with age inversely correlated.
Conclusion(s): Doses of postoperative sedation and analgesia are not correlated with patient race, ethnicity, and language. Factors associated with differences in medication doses are likely reflective of postoperative acuity. Standardized protocols utilized at this center may protect against and eliminate bias previously described. Future research should support development and implementation of protocols in other settings to eliminate bias and reduce in-hospital disparities.