Allergy, Immunology and Rheumatology
Session: Allergy, Immunology, and Rheumatology
570 - With Equitable Treatment Children With Down Syndrome-Associated Arthritis Have Better Outcomes Compared to Juvenile Idiopathic Arthritis
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 570
Publication Number: 570.381
Publication Number: 570.381

Irene Chern, MD (she/her/hers)
Pediatrics Resident Physician
St. Christopher's Hospital for Children
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Down syndrome (DS) is one of the most common genetic disorders affecting approximately 1 in 1000 live births globally. DS is a chromosomal disorder caused by imbalanced genes on chromosome 21 which results in an increased incidence of autoinflammatory and autoimmune conditions. Individuals with DS have a significantly higher prevalence of inflammatory arthritis, termed Down Syndrome-associated arthritis (DA), compared to the general population. Additionally, there is a significant delay in diagnosis of DA compared to juvenile idiopathic arthritis (JIA), which is the most encountered pediatric rheumatic disease. Additional research is needed to improve the care of individuals with DA to better elucidate the similarities and differences between DA and JIA, which may lead to earlier diagnosis and treatment.
Objective: This study compares the clinical presentation and outcomes between DA and JIA in the Pediatric Rheumatology Care & Outcomes Improvement Network (PR-COIN) registry.
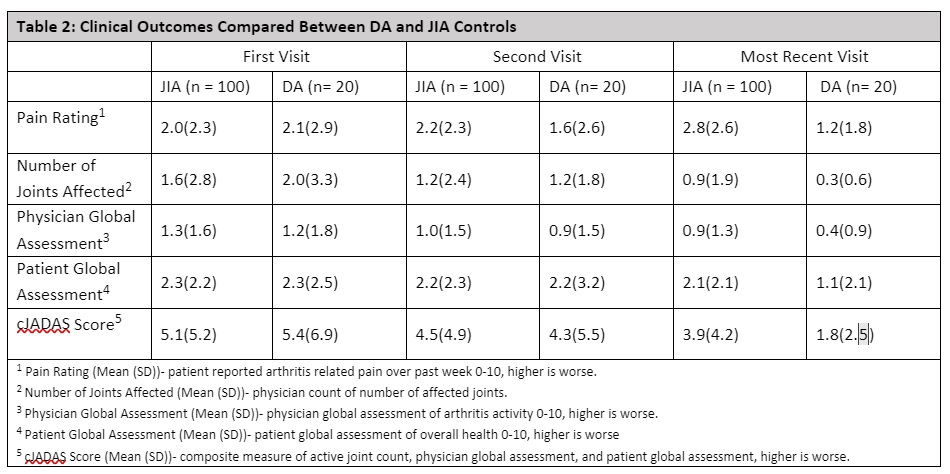
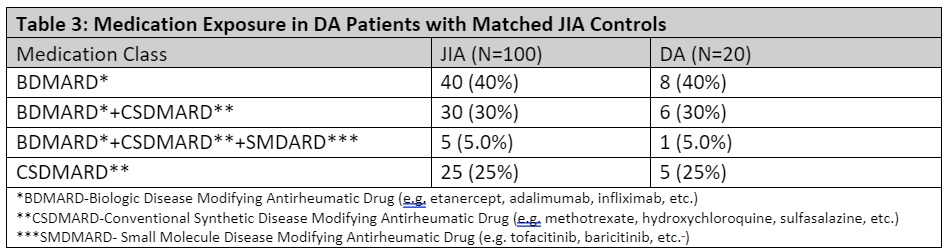
Design/Methods: Using the PR-COIN registry, a retrospective case-control study evaluated patients with DA that were matched to patients with JIA. Patients were matched on age, gender, arthritis subtype, and medication exposure. Clinical juvenile arthritis disease activity scores (cJADAS), which are a composite measure of active joint count as well as physician and patient global assessments, were compared between DA and JIA groups.
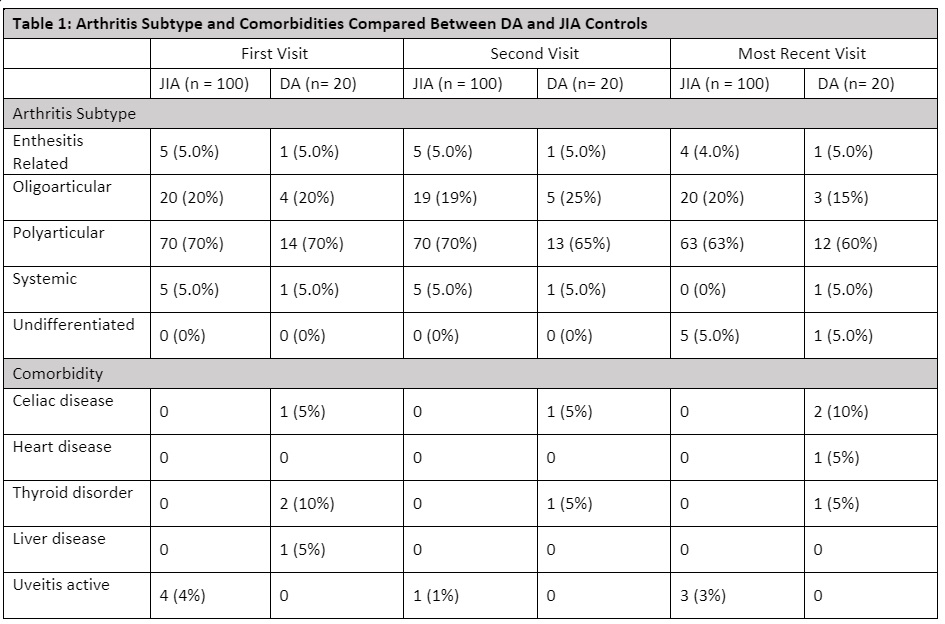
Results: Twenty patients with DA and 100 with JIA were identified. The mean days between first and last visits were 1157 for patients with JIA and 1664 for DA. Those with DA had more comorbid autoimmune conditions, but less uveitis compared to the JIA group (Table 1). At the last visit those with DA had lower cJADAS scores compared to the JIA group. Compared to the JIA group, the DA group had an average pain score that improved over time whereas the JIA group had a pain score that increased over time (Table 2). The medication distribution and exposure were the same between groups (Table 3).
Conclusion(s): While a delay in diagnosis of DA is not uncommon, this study suggests that with appropriate treatment patients with DA can have similar clinical outcomes compared to those with JIA. This study also shows that those with DA report less pain compared to those with JIA and reported pain tracked with active disease for those with DA, but not JIA. We also see more comorbidities, but no uveitis for those with DA. These findings illustrate the importance of early disease recognition and treatment for those with DA to minimizes morbidity and promote equity in patient outcomes.