Nephrology
Session: Nephrology 3
3 - Association of AKI by ICD-10 code with blood pressure severity, target organ injury, and obesity, dyslipidemia, and hyperglycemia at baseline in youth referred to pediatric hypertension subspecialists
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 3
Publication Number: 3.2030
Publication Number: 3.2030

Mital Patel, MD (she/her/hers)
Assistant Professor
Wake Forest Baptist Health - Brenner Children's Hospital
Winston-Salem, North Carolina, United States
Presenting Author(s)
Background: Acute kidney injury (AKI) is a well-studied risk factor for new onset hypertension. Cardiovascular risk factors including baseline blood pressure severity, target organ injury (TOI), obesity, dyslipidemia, and hyperglycemia are heterogenous at the time of hypertension diagnosis. It is unclear if these baseline factors are different in youth with a history of AKI compared to those who do not have a history of AKI.
Objective: Assess the difference in cardiovascular risk factors at the time of index visit for hypertension in youths affected by AKI compared to those not affected by AKI.
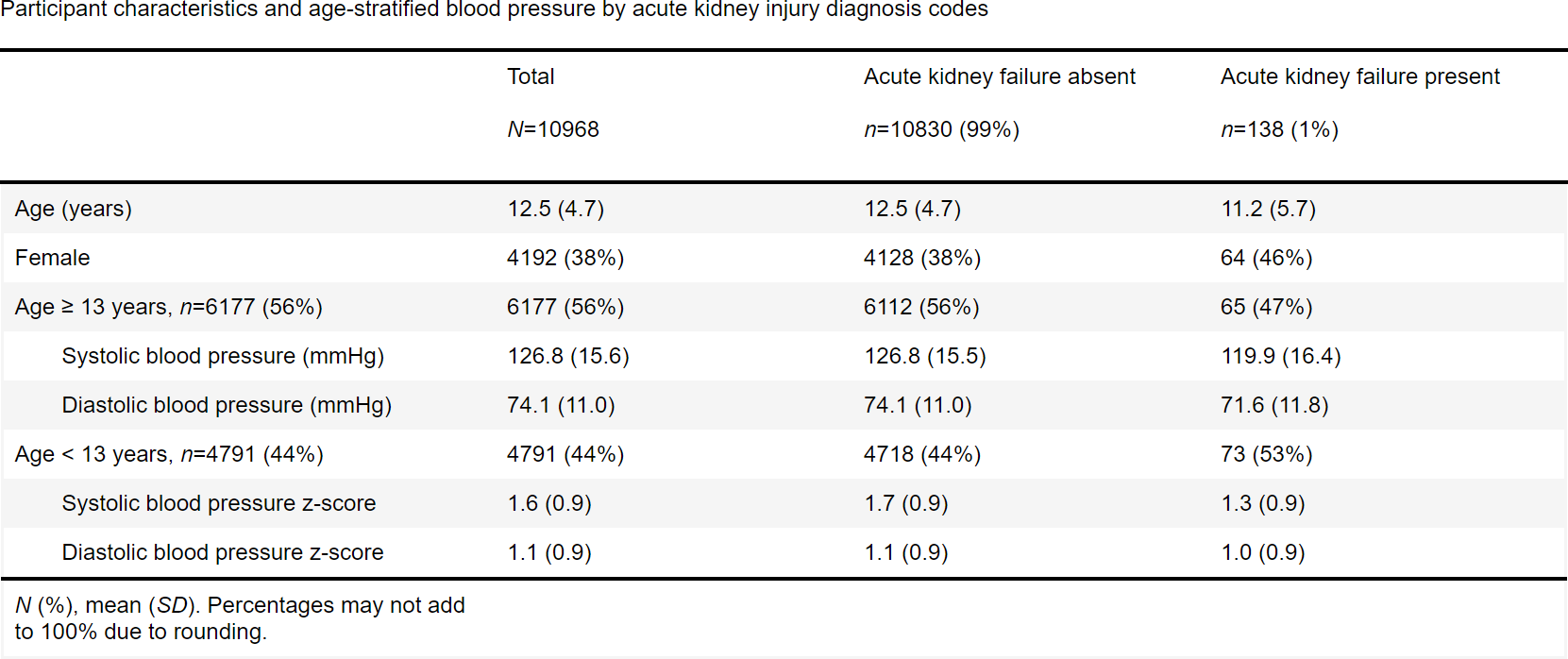
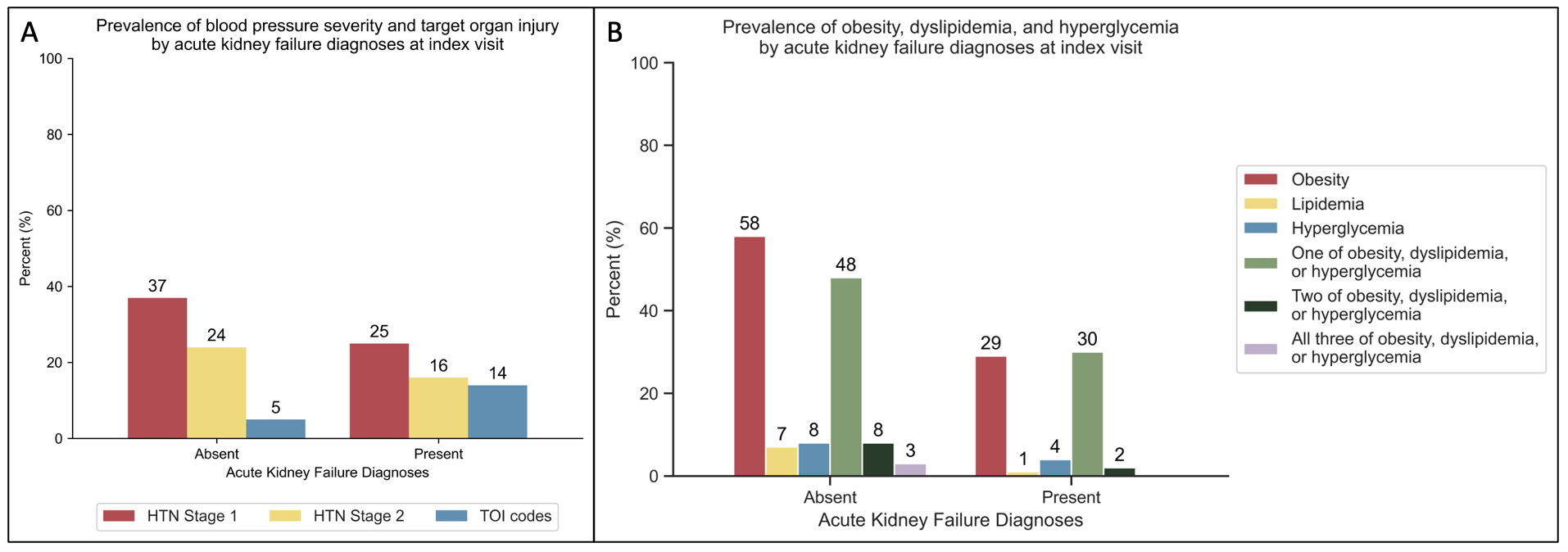
Design/Methods: Cross-sectional analysis of baseline data from participants in the Study of the Epidemiology of Pediatric Hypertension (SUPERHERO), a large multisite registry of youth under 19 years of age referred to hypertension subspecialty clinics across 8 sites. Our exposure was AKI defined by ICD-10 code (e.g., N17.X) at index visit. Our outcomes were blood pressure severity (based on age-appropriate national guidelines), obesity by body mass index or weight-for-length percentiles per national guidelines, and TOI to heart or kidney, hyperglycemia, or dyslipidemia all by ICD-10 codes. We used multivariable generalized linear models.
Results: 10,968 youth were included in the study. Within this cohort, 138 (1%) had a diagnosis of AKI. Adolescents with AKI diagnosis code had 5.5 mm Hg lower systolic blood pressure and children with AKI diagnosis code had -0.27 lower systolic blood pressure z-score. Blood pressure severity classification was lower at all ages (Table 1). Youth with AKI had 45% lower risk of obesity, 78% lower risk of dyslipidemia, and lower number of cardiovascular health risk factors (Table 2). Youth with AKI diagnosis code had 175% higher risk of TOI (adjusted RR 2.75, 95% CI 1.75-4.3) (Table 2).
Conclusion(s): In this large, multisite cohort of youth referred for hypertension disorders, those with a diagnosis code for AKI had higher risk of TOI at index visit despite lower blood pressure severity and better cardiovascular health. This study suggests that youth with a history of AKI require closer monitoring for early detection of TOI. Limitations of our study include use of administrative diagnosis codes to identify AKI which has been associated with lower inclusion of patients with stage 1 AKI. Future studies should include a more inclusive definition of AKI with use of creatinine and urine output-based definitions.