Emergency Medicine
Session: Emergency Medicine 10: Trauma
403 - Standardization of Discharge Instructions for Mild Traumatic Brain Injury/Concussion in Children Presenting to ED: A Quality Improvement Project
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 403
Publication Number: 403.2989
Publication Number: 403.2989

Niralee K. Rana, BS (she/her/hers)
Research Associate
Weill Cornell Medicine
Clifton, New Jersey, United States
Presenting Author(s)
Background: Mild traumatic brain injuries (mTBI) or concussions account for high rates of emergency department (ED) visits. Concussion diagnoses are used less often in young children leading to a variability in parental education and discharge instructions. Lack of discharge guidance may increase parental anxiety, impact recovery, and increase ED visits.
Objective: To increase the proportion of ED patients discharged with age-appropriate instructions for mTBI to 50% by June 1, 2024.
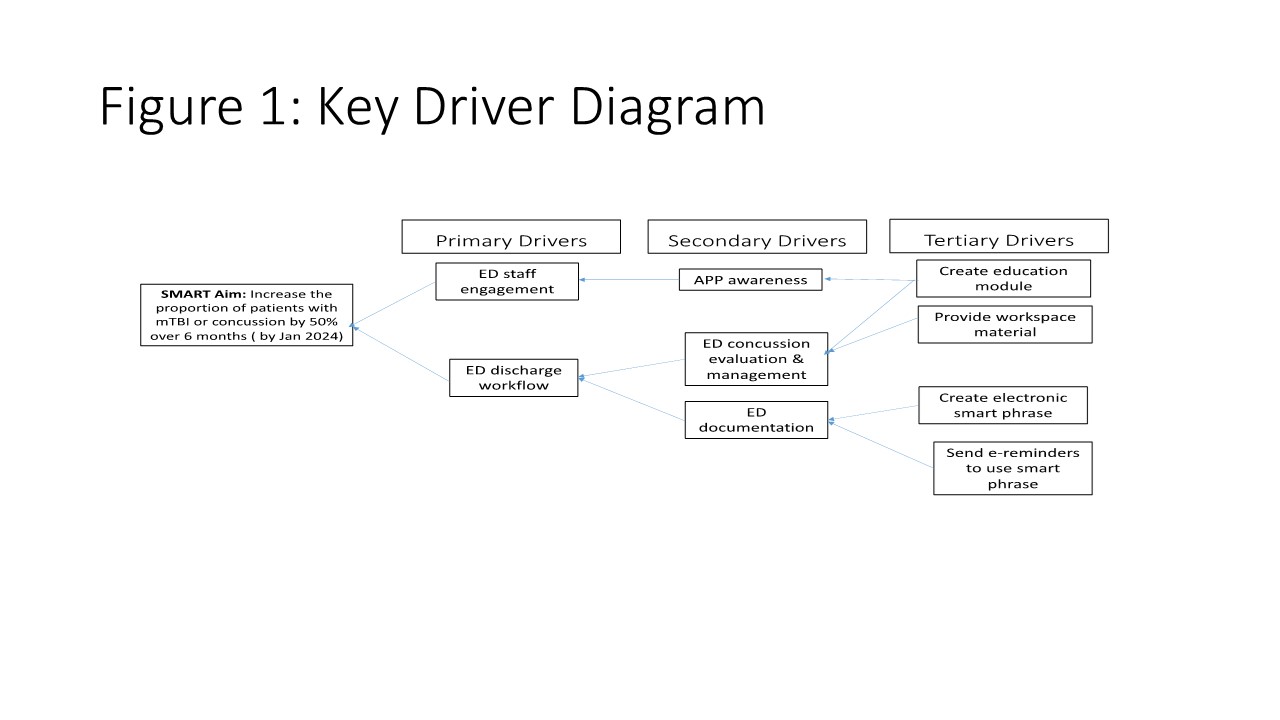
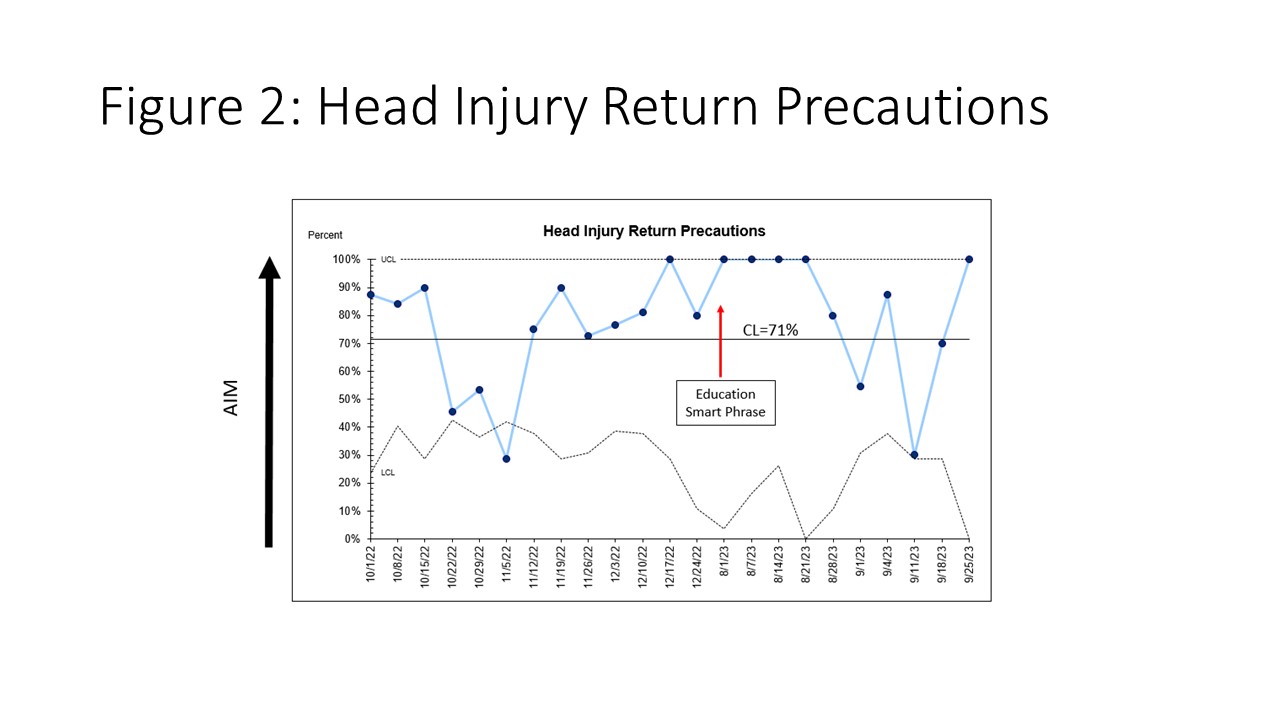
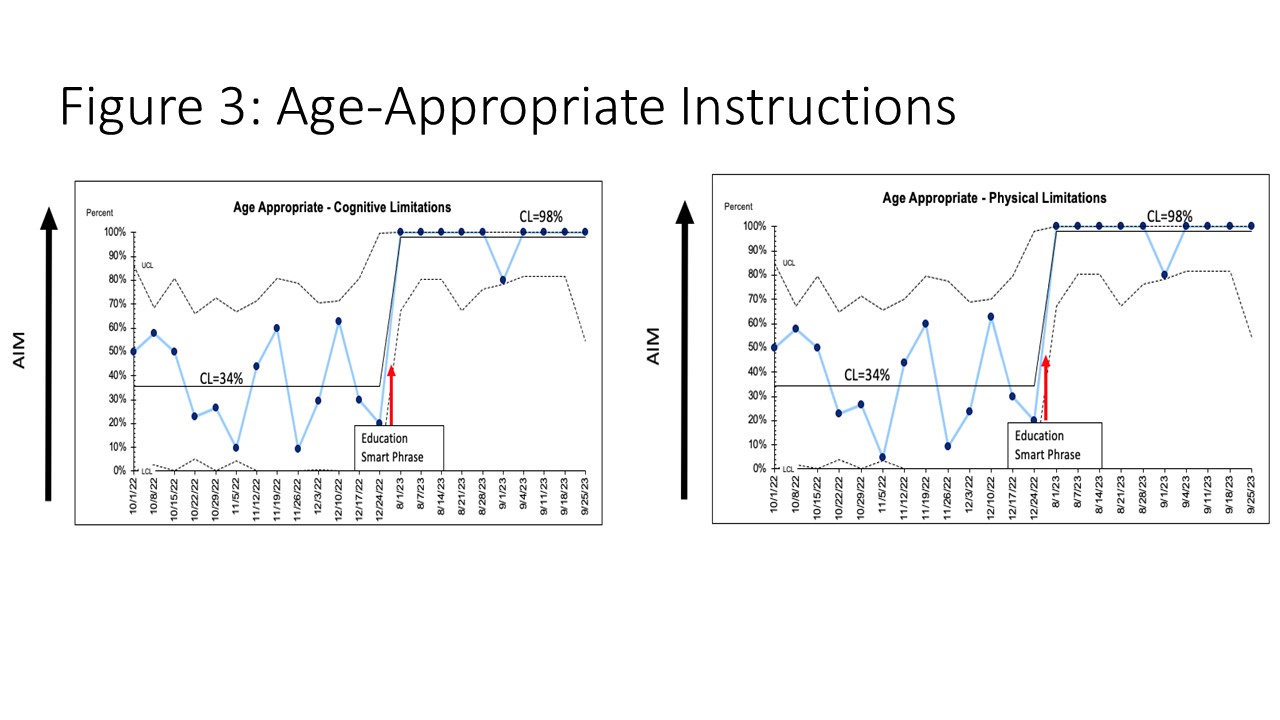
Design/Methods: This observational time series with planned sequential experimentation is in progress at a Pediatric ED affiliated with an urban academic medical center from October 2022- June 2024. All pediatric ED patients aged 0-18 years with mTBI or concussion associated ICD-10 codes were included. An interdisciplinary team including ED faculty, pediatric neurology, nursing, clinical informatics, and QI specialist developed the key driver diagram (Fig 1). Interventions derived from tertiary drivers included ED staff education and creation of an electronic medical record (EMR) smart phrase of standardized discharge instructions for mTBI or concussion for children ages 0-5 years and ≥ 6 years based on CDC guidelines and expert consensus. Data were collected via EMR review. Our process measures included percentage of patients who received discharge instructions with 1) head injury specific precautions, 2) cognitive and 3) physical limitations, age-appropriate instructions related to 4) cognitive and 5) physical limitations and 6) clinical diagnosis of concussion. Our balancing measures include head CT utilization. Data were displayed and analyzed using statistical process control “P” charts and API rules were applied to detect special cause variation.
Results: In this study of 256 patients, 71% of patients received head injury specific precautions discharge instructions (Fig 2), 48% received information about cognitive and physical limitations and 30% had a diagnosis of concussion. We observed an improvement in the percentage of patients who received age-appropriate instructions for both cognitive and physical limitations from 38% to 98% over the start of our first PDSA cycle (Fig 3). There was no increase in head CT utilization.
Conclusion(s): Creating age-appropriate standardized EMR discharge smart phrases for physical and cognitive recovery led to increased incorporation of these discharge instructions from the Pediatric ED. Next steps include analyzing our data by race, ethnicity and language as well as assessing the impact of our interventions on parental anxiety.