Neonatology
Session: Neo-Perinatal Health Care Delivery 2: Epidemiology/Health Services Research
332 - Maternal and neonatal outcomes of unintended pregnancies among women experiencing homelessness in the United States- a population-based study.
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 332
Publication Number: 332.1316
Publication Number: 332.1316
- RS
Rashmi Priya Somu, M.B.B.S, MD (she/her/hers)
Neonatology fellow
Harbor UCLA Medical Center
Torrance, California, United States
Presenting Author(s)
Background: Housing status and pregnancy intention are crucial social determinants of health that influences perinatal morbidity independently. Previous studies have explored the association between housing instability and adverse perinatal outcomes. However, the impact of unintended pregnancies as a predictor of maternal and neonatal morbidity among women experiencing homelessness (WEH) and their domiciled counterparts are not well known.
Objective: To examine the incidence rate of unintended pregnancies among WEH, compare with their domiciled counterparts and evaluate the adverse neonatal and maternal outcomes using Pregnancy Risk Assessment Monitoring System (PRAMS) data from 2004-2021.
Design/Methods: PRAMS is a surveillance project of the Centers for Disease Control and Prevention (CDC). PRAMS surveillance includes 81% of all live births in the United States.
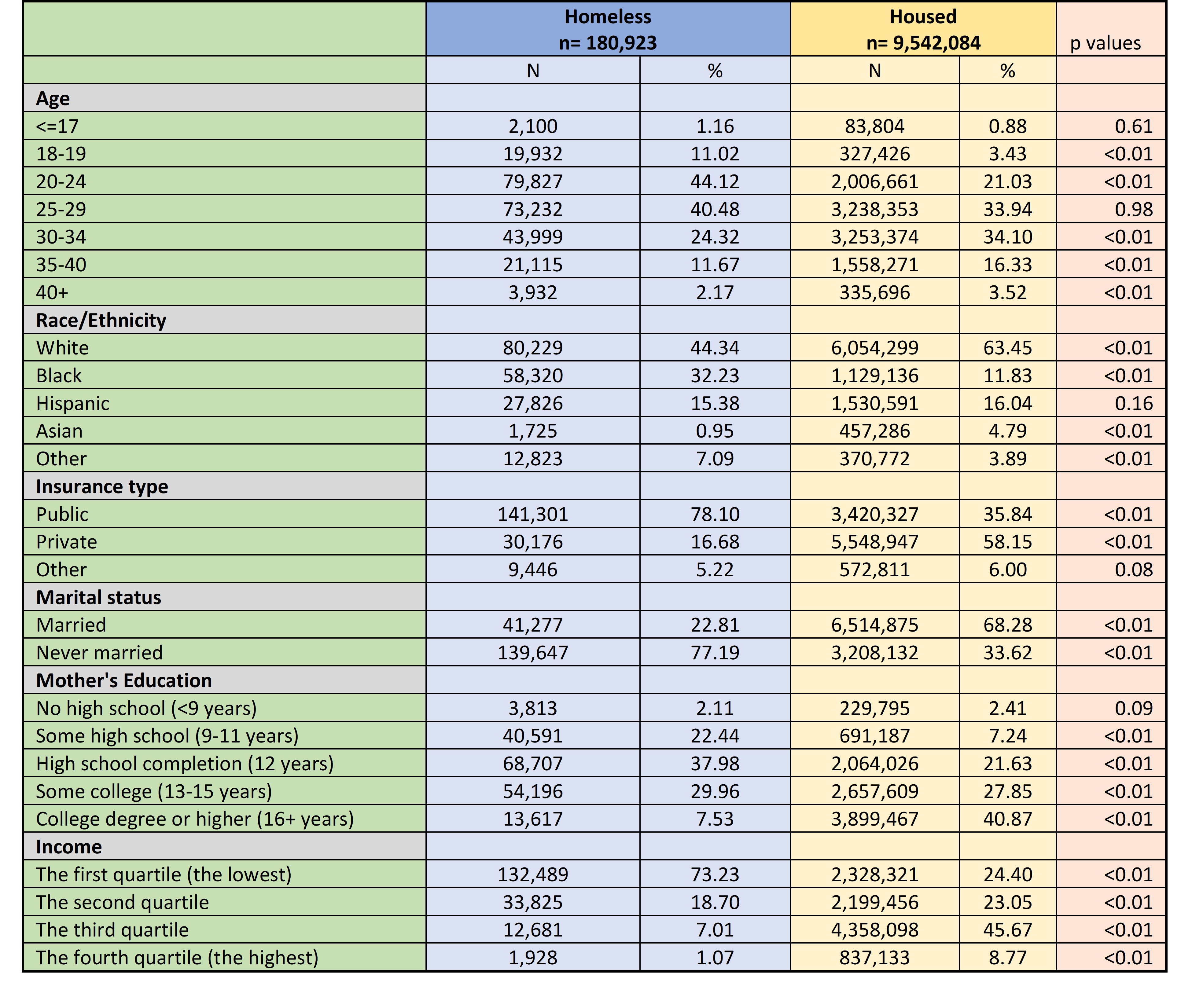
Multivariable logistic regression models were used to assess the associations of homelessness with postpartum depression, attendance of postpartum care, low birth weight, and preterm birth. The models were adjusted for age, race, ethnicity, insurance type, marital status, education, and income quartile (Table 1).
Results: A total of 652,295 postpartum women were included in the database. After excluding responses missing homelessness and pregnancy intention, 164,403 were included in the final analytical cohort. Of which 3,806 were experiencing homelessness that accounts to 2.3 % of our analytical cohort. WEH had higher odds of unintended pregnancies compared to their domiciled counterparts (adjusted odds ratio [aOR] 1.65, 95 % confidence interval [CI] 1.47-1.84, p value [p] < 0.01).
We found statistically significant association of unintended pregnancy with increased odds of postpartum depression (aOR 1.27, 95 % CI 1.20- 1.35, p < 0.01), attendance of postpartum care (aOR 1.08, 95 % CI 1.01- 1.16, p < 0.05), low birth weight (aOR 1.16, 95 % CI 1.11-1.22, p < 0.01), and preterm birth (aOR 1.13, 95 % CI 1.06- 1.20, p < 0.01) among domiciled women. However, no such associations were detected among WEH, which could be due to the small sample size (Table 2).
Conclusion(s): Our study highlights a significant association of unintended pregnancy with adverse perinatal outcomes among domiciled women, while we failed to detect these associations among WEH, possibly due to the limited sample size in this vulnerable and under-researched population. To better understand the dynamics within WEH, further research with larger sample sizes is essential, focusing on comprehensive studies to address the unique challenges faced by this demographic.
.jpg)
