Medical Education
Session: Medical Education 5
409 - Integrating a Validated Structured Observational Tool That Incorporates Entrustable Professional Activities (EPAs) into the Pediatric Continuity Clinic
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 409
Publication Number: 409.1308
Publication Number: 409.1308

Grace E. Black, MD
Associate Professor of Pediatrics
University of Rochester
Rochester, New York, United States
Presenting Author(s)
Background: Primary care education of pediatric residents includes didactic and hands on learning in the weekly continuity clinic. Busy clinic preceptors have limited time to observe residents’ clinical encounters and provide timely and actionable feedback on clinical interactions that are components of EPAs of the American Board of Pediatrics (ABP). Overcoming these barriers is important because the ABP plans to integrate EPAs into the credentialing process for ABP initial certification exams by 2028.
Objective: 1. To implement use of a Structured Clinical Observation (SCO) tool in resident continuity clinic.
2. To assess feasibility and acceptability of use of the EPA 5 supervision scale (“Provide a Medical Home for Children of All Ages”) in the clinic setting.
Design/Methods: Prior to the start of the 2023-24 academic year, we created a schedule for faculty to observe one resident per continuity clinic day. A faculty member observed the resident for an entire patient encounter and completed the SCO tool, which was modeled on a validated tool (Howe and colleagues, presented at PAS 2023) that included the EPA 5 supervision scale. Additionally, faculty provided immediate direct feedback to the resident. Completed SCO forms were uploaded to the residency evaluation system for ongoing review by residents and use in residency program Clinical Competency Committee evaluations. Faculty were surveyed after completing a round of resident observations.
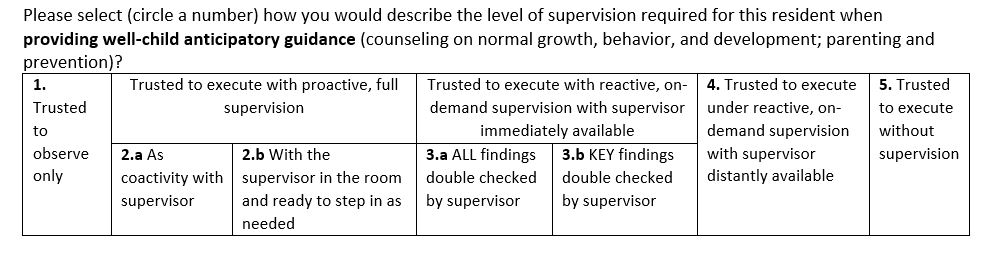
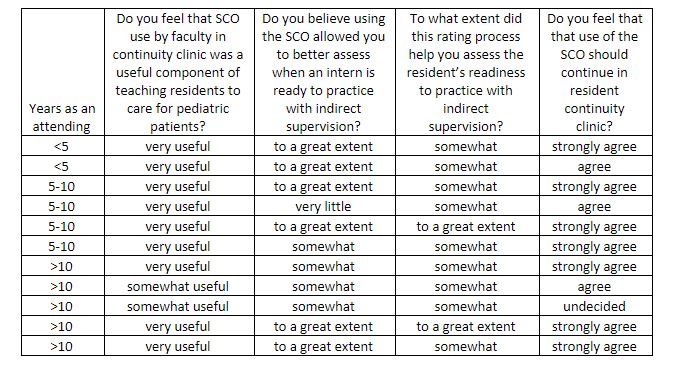
Results: In the 2023-24 academic year, 14 faculty members observed 21 pediatric residents over 2 months. Mean duration of observations was 25 minutes; mean duration of oral feedback sessions was 5 minutes. Scores on the EPA supervision scale ranged from 2.b for interns to 5 for senior residents (scale in Figure 1). Eleven faculty members completed follow-up surveys; 9 (82%) felt that the SCO was very useful as a component of teaching residents to care for pediatric patients, while the remaining 2 (18%) felt it was somewhat useful. Ten faculty strongly agreed/agreed the observations should continue, with 1 faculty undecided. See Table 1 for additional results.
Conclusion(s): Direct observations using a SCO tool that integrated EPA 5 was a feasible and helpful way to provide necessary feedback to residents in continuity clinic and meet the ABP’s anticipated requirement for integration of EPAs into resident assessment. We anticipate that routine use of scheduled, direct observations will be an ongoing part of our continuity clinic evaluation process for pediatric residents.