Hypertension
Session: Hypertension
62 - Association of Preterm Birth, Low Birth Weight, and Growth Restriction with Baseline Blood Pressure Severity, Target Organ Injury, and Cardiovascular Health
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 62
Publication Number: 62.2050
Publication Number: 62.2050

Margaret Murphy, PhD, RD (she/her/hers)
Assistant Professor/Pediatric Renal Dietitian
University of Kentucky College of Medicine
University of Kentucky Healthcare
Lexington, Kentucky, United States
Presenting Author(s)
Background: Survival following premature birth in the US has steadily improved in recent decades, as has the prevalence of youth-onset hypertension (HTN). The association of preterm birth, low birth weight (LBW), and small for gestational age (SGA) with HTN has been observed; however, little is known how these early-life factors impact cardiovascular risk once an individual develops HTN .
Objective: Investigate the relationships between preterm birth, LBW, and SGA in relation to blood pressure (BP) severity, target organ injury (TOI), and cardiovascular health in youth with HTN disorders.
Design/Methods: Cross-sectional analysis of baseline data from the Study of the Epidemiology of Pediatric Hypertension (SUPERHERO) Registry, a multisite retrospective cohort of youth referred to subspecialty care for hypertension disorders using electronic health record data. Inclusion criteria were an initial subspecialty clinic visit for hypertension disorders identified by ICD-10 codes from 1/1/2016–12/31/2022 and age < 19 years. Exclusion criteria were kidney failure on dialysis, kidney transplantation, or pregnancy by ICD-10 codes. Exposures included preterm birth, LBW, and SGA identified by ICD-10 codes. Adjusted generalized linear models estimated the association of preterm birth, LBW, and SGA with the outcomes of BP severity with z-scores and classification per US guidelines, obesity by BMI or weight-for-length percentiles, and TOI, dyslipidemia, and hyperglycemia by ICD-10 codes.
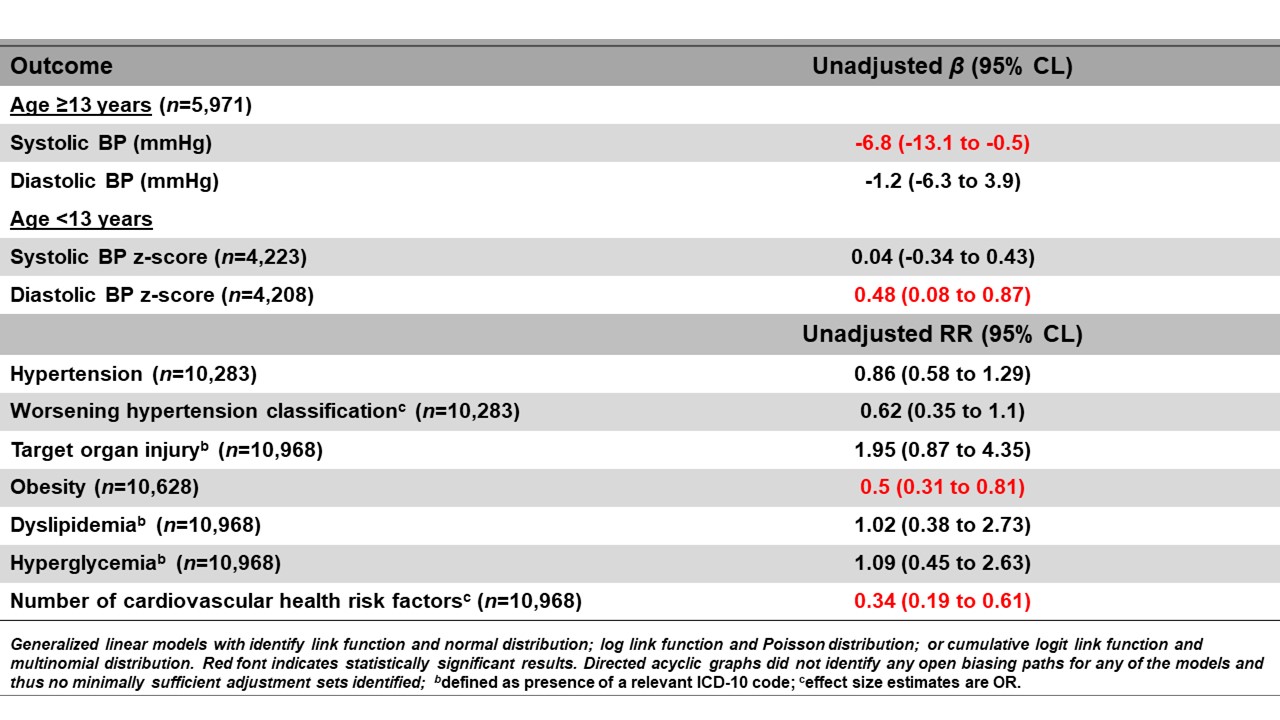
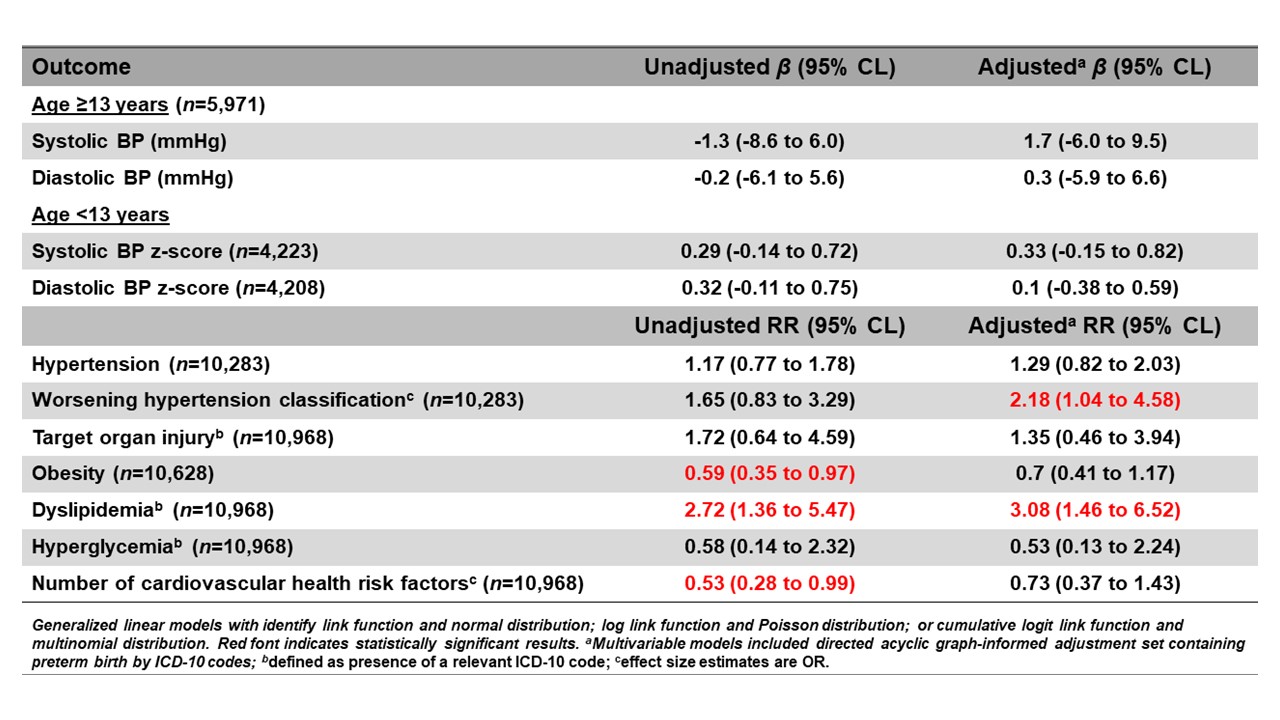
Results: Of the 10,968 participants, the mean age was 12.5 ±4.7, 38% were female, < 1% (n=57) had preterm birth, < 1% (n=43) had LBW, and < 1% (n=17) SGA. Participants with preterm birth had 50% lower risk of obesity and cardiovascular risk health factors (OR 0.34 , CL: 0.19 to 0.61). Participants with LBW had worse BP severity (RR 2.18, CL 1.04 to 4.58) and a 3-fold higher risk of dyslipidemia (CL: 1.46 to 6.52). Despite less BP severity, participants with SGA had higher risk of TOI (RR: 3.26, CL 1.05 to 10.13).
Conclusion(s): In a large multisite cohort of youth referred for HTN disorders, participants with preterm birth had a lower risk of obesity and cardiovascular risk factors; however, participants with LBW had heightened risk of BP severity and dyslipidemia despite a lower risk of obesity. Interestingly, SGA was associated with a greater risk of TOI without greater risk of obesity or BP severity. Future studies will investigate these associations with laboratory and echocardiogram data to inform future management of youth with HTN disorders beginning in early life.
.jpg)
