Infectious Diseases
Session: Infectious Diseases 1
571 - Antibiotic Overuse in Pediatric Patients Hospitalized with RSV, COVID-19, and Influenza
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 571
Publication Number: 571.424
Publication Number: 571.424

Mrinmoyee C. Kalasikam (she/her/hers)
Undergraduate student
Vanderbilt University School of Medicine
Brentwood, Tennessee, United States
Presenting Author(s)
Background: Children hospitalized with viral respiratory tract infections (RTIs) are often treated with antibiotics due to concern for bacterial co-infection. However, many children with viral RTIs do not have concurrent bacterial infections, so this practice leads to unnecessary antibiotic treatment. This can, in turn, lead to development of resistant bacteria and adverse events. Unlike in adults, the extent of antibiotic overuse in hospitalized children with community-onset viral RTI has not been well-quantified in recent years and may have worsened during the COVID-19 pandemic.
Objective: The objectives of this study were to quantify the extent of antibiotic overtreatment and to determine predictors of antibiotic use among a contemporary cohort of children hospitalized with various viral RTIs.
Design/Methods: We performed a single center retrospective study evaluating percentages of antibiotic use and bacterial co-infection among children and adolescents aged < 19 years old, hospitalized with primary diagnosis of respiratory syncytial virus (RSV), Influenza, or SARS-CoV-2 between April 2020 and May 2023. A true infection was defined as a growth of clinically significant bacteria from any specimen source, including blood, urine, pleural fluid, cerebrospinal fluid, and respiratory secretions. Patients were identified by diagnosis codes, and their medical records were reviewed to collect demographic and clinical characteristics. Finally, predictors of antibiotic treatment were determined using multivariable logistic regression to compare antibiotic utilization by virus type.
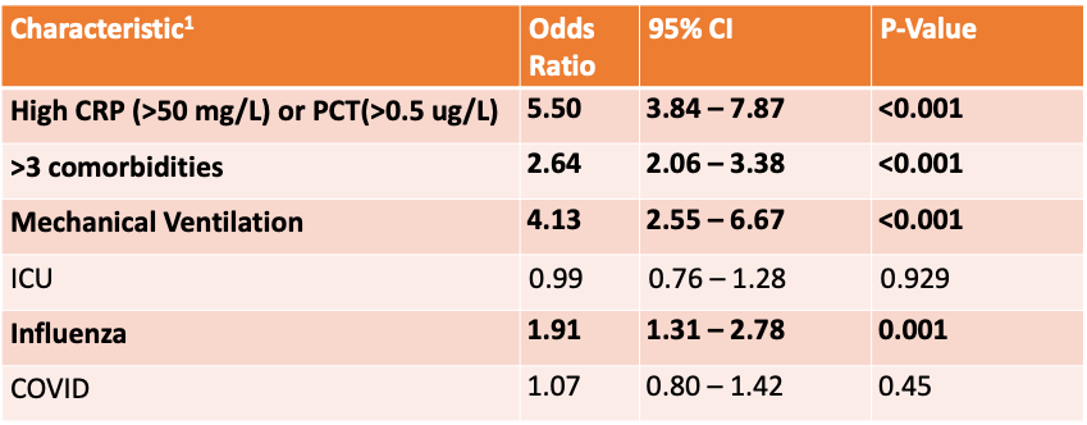
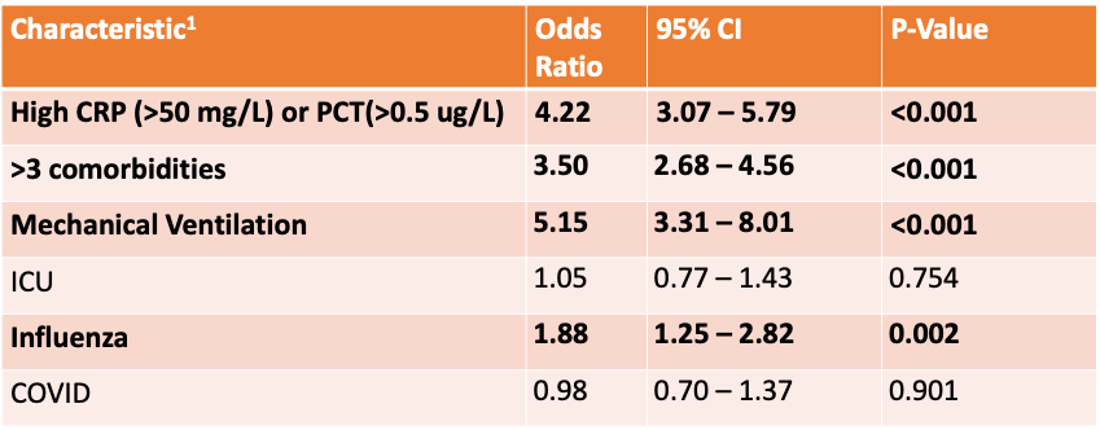
Results: Median age was lowest for RSV patients and highest for COVID-19 patients. Though COVID-19 patients had the greatest proportion of culture-confirmed bacterial co-infections (10.3%), influenza patients received the greatest proportion of antibiotics (60.6%, p < 0.001). Independent predictors for receiving any duration of antibiotics and receiving >3 days of antibiotics were high inflammatory markers (C-reactive protein or procalcitonin), having >3 comorbidities, mechanical ventilation, and influenza diagnosis. Patients with elevated inflammatory markers were significantly more likely to receive antibiotics than those without elevated inflammatory markers (OR 5.50, 95% CI 3.84 to 7.87) when adjusted for age, race, >3 comorbidities, mechanical ventilation, and influenza.
Conclusion(s): Antibiotic treatment percentages in children hospitalized with community-onset viral RTIs are significantly higher than the burden of culture-confirmed bacterial infection in this population. These data can be used to promote more judicious antibiotic use.
.png)