Medical Education
Session: Medical Education 6
420 - De-Escalation of the Agitated Pediatric Patient: A Standardized Patient Case for Pediatric Residents
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 420
Publication Number: 420.1282
Publication Number: 420.1282
- DA
Daniel Alanko, MD (he/him/his)
Resident Physician
Hasbro Children's Hospital at Rhode Island Hospital
Bloomfield, New Jersey, United States
Presenting Author(s)
Background: There has been a recent increase in pediatric mental health emergencies, outpacing the supply of psychiatric resources and ultimately leading to increased inpatient “boarding” of patients requiring psychiatric admission. Pediatric trainees must learn the skills to effectively de-escalate a patient with unsafe behavior, as their patients have increasingly complex mental health needs. Only a minority of pediatric residents report high levels of perceived competence in the assessment and treatment of mental health conditions. To maintain safety and provide the best possible care to these patients, resident education must keep up with changing demands. Simulation can provide high-fidelity practice in a safe environment, adding to existing literature mostly surrounding lecture- and case-based mental health education.
Objective: The objective of this standardized patient (SP) case was to increase resident confidence in assessing situational safety, verbal de-escalation techniques, and timing and selection of appropriate pharmacologic therapy for an acutely agitated pediatric patient. These goals were chosen with the aim of improving staff and patient safety and overall care in the setting of an inpatient behavioral health crisis.
Design/Methods: Resident learners were presented with a teenage patient, played by a trained SP, who became acutely agitated with aggressive behaviors while admitted and awaiting transfer to a psychiatric facility. Learners were expected to attempt verbal de-escalation, followed by an appropriate pharmacologic therapy if indicated. A standardized debrief was conducted with the assistance of pediatric mental health experts. Learners were surveyed to obtain feedback on the session.
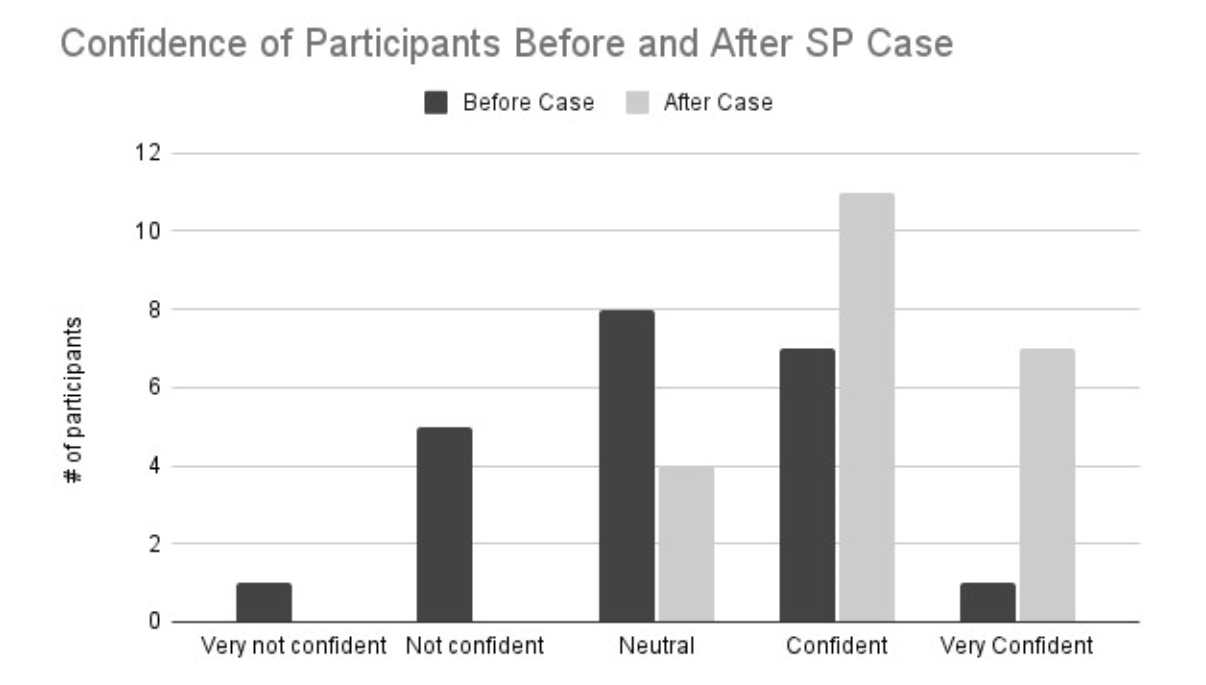
Results: Twenty-two learners participated in this educational activity. Resident confidence in their management of the acutely agitated pediatric patient significantly increased after completion of the session (Figure 1). Seventy-three percent of learners felt confident or very confident in their de-escalation skills at the end of the case, and eighty-six percent agreed that the case improved their confidence in managing acute agitation scenarios on the inpatient wards.
Conclusion(s): This case fills an important gap in pediatric resident education and led to overall increased resident confidence in caring for the acutely agitated pediatric patient. Future iterations of the case may include multidisciplinary learners at various levels of training and may include evaluating changes in patient-centered outcomes, such as restraint use, after implementation of this curriculum.