General Pediatrics
Session: General Pediatrics 3
354 - What's in that Ear, Identifying Gaps in Self-Efficacy and Current Practice to Develop an Innovative Solution for Managing Acute Otitis Media using the Digital Otoscope
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 354
Publication Number: 354.1277
Publication Number: 354.1277

Betty Del Rio Rodriguez, MD, MPH (she/her/hers)
Assistant Professor of Pediatrics
Baylor College of Medicine
Pasadena, Texas, United States
Presenting Author(s)
Background: Acute otitis media (AOM) is a leading cause of misdiagnosis and antibiotic over prescription in primary health clinics, despite clear American Academy of Pediatrics (AAP) guidelines. Misdiagnosis and over prescription can be attributed to challenging ear examination, gaps in knowledge, self-efficacy and communication skills of primary care providers. We seek to address these challenges with an innovative intervention using the digital otoscope
Objective: To define the areas of need for a comprehensive multi-faceted intervention to improve diagnostic accuracy and management of children with AOM in clinic setting.
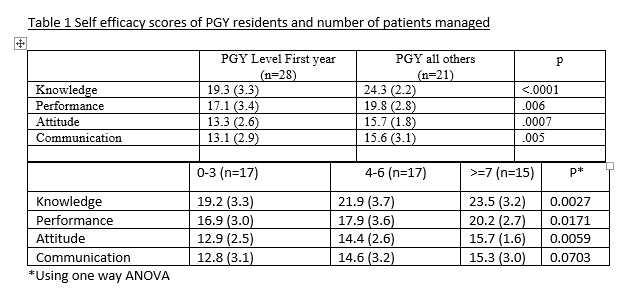
Design/Methods: Data extraction tool was utilized for retrospective chart review of patients with AOM across 2 primary care clinics for a 3-month period. Through iterative process we developed a 22-item self-efficacy (SE) survey and designed a blended curriculum (Fig.1) comprised of asynchronous microteaching modules (EdApp) with knowledge assessment with gamification elements for learner engagement. 2 didactic lectures covered AAP guidelines and hands-on-skill demonstration for utilizing the digital otoscope for examination and for effective patient communication. We used the t-test and ANOVA to analyze mean group differences in the SE survey.
Results: Pre-intervention chart review (n=46) provided descriptive data (Table 1 ) demonstrating 46% of patients with AOM met AAP criteria for diagnosis. Of the 54% that did not meet criteria, 77% received a wrong diagnosis, lacking documentation for history in 55% and incomplete physical exam in 36%. We collected 49 baseline SE survey responses showing PGY1’s reporting significantly lower scores across all 4 parameters (Table 2). PGY2/ 3 residents reported higher SE scores after managing more patients. Residents reported lowest scores for knowledge of ear exam findings, indications for starting antibiotics, maneuvering pinna to visualize ear canal, ability to reposition the child and patient communication strategies for watchful waiting when deferring antibiotics. 42 residents scored 76% on knowledge assessment while winning 200+ points on the leaderboard, completing the asynchronous module in 12 minutes.
Conclusion(s): Our preliminary data identified inaccurate diagnosis of AOM, with a large number lacking documentation supporting the diagnosis and highlighted areas for standardizing documentation. SE survey highlighted the need to address gaps in knowledge and examination skills training of learners. In the future, we will assess patient satisfaction and effectiveness of our intervention with patient outcome data.
.png)
.png)