Hypertension
Session: Children with Chronic Conditions 3
286 - Association of Insurance Status and Individual-level Social Risk Factors by ICD-10 Codes with Blood Pressure Severity, Target Organ Injury, and Cardiovascular Health at Baseline
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 286
Publication Number: 286.441
Publication Number: 286.441

Estefania G. Narvaez, BS (she/her/hers)
Incoming Medical Student
Atrium Health Wake Forest Baptist
Waxhaw, North Carolina, United States
Presenting Author(s)
Background: Youth with hypertension (HTN) are susceptible to immediate and enduring adverse cardiovascular (CV) health outcomes, especially those from disadvantaged backgrounds who may face even greater risks. However, the impact of health disparities and related factors like insurance status and individual-level social risk factors is not well-defined.
Objective: To determine if insurance status and individual-level social risk factors are associated with differences in baseline blood pressure (BP) severity, target organ injury (TOI), and CV health in youth with HTN disorders.
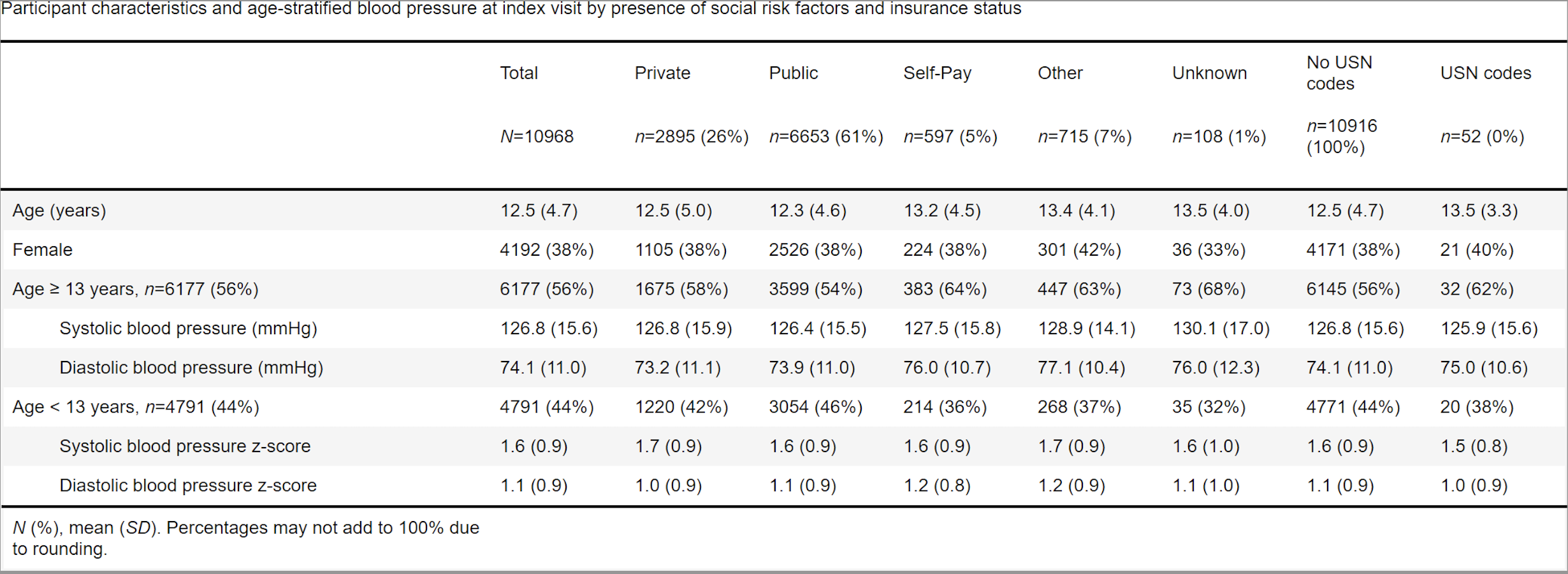
Design/Methods: Cross-sectional analysis of baseline data from the Study of the Epidemiology of Pediatric Hypertension (SUPERHERO), a multisite retrospective registry of youth referred to subspecialty care for HTN disorders using electronic health record data validated with manual record review. Inclusion criteria were initial visit for HTN disorder identified by ICD-10 codes from 1/1/2015 to 12/31/2022 and age < 19 years. Exclusion criteria were kidney failure on dialysis, kidney transplantation, or pregnancy by ICD-10 codes. Exposures were insurance status and individual-level social risk factors defined by ICD-10 codes. The outcomes were BP and related z-scores, BP classification per national guidelines, TOI by ICD-10 codes, and CV health by ICD-10 codes (obesity by percentiles) at the index visit. We used generalized linear models.
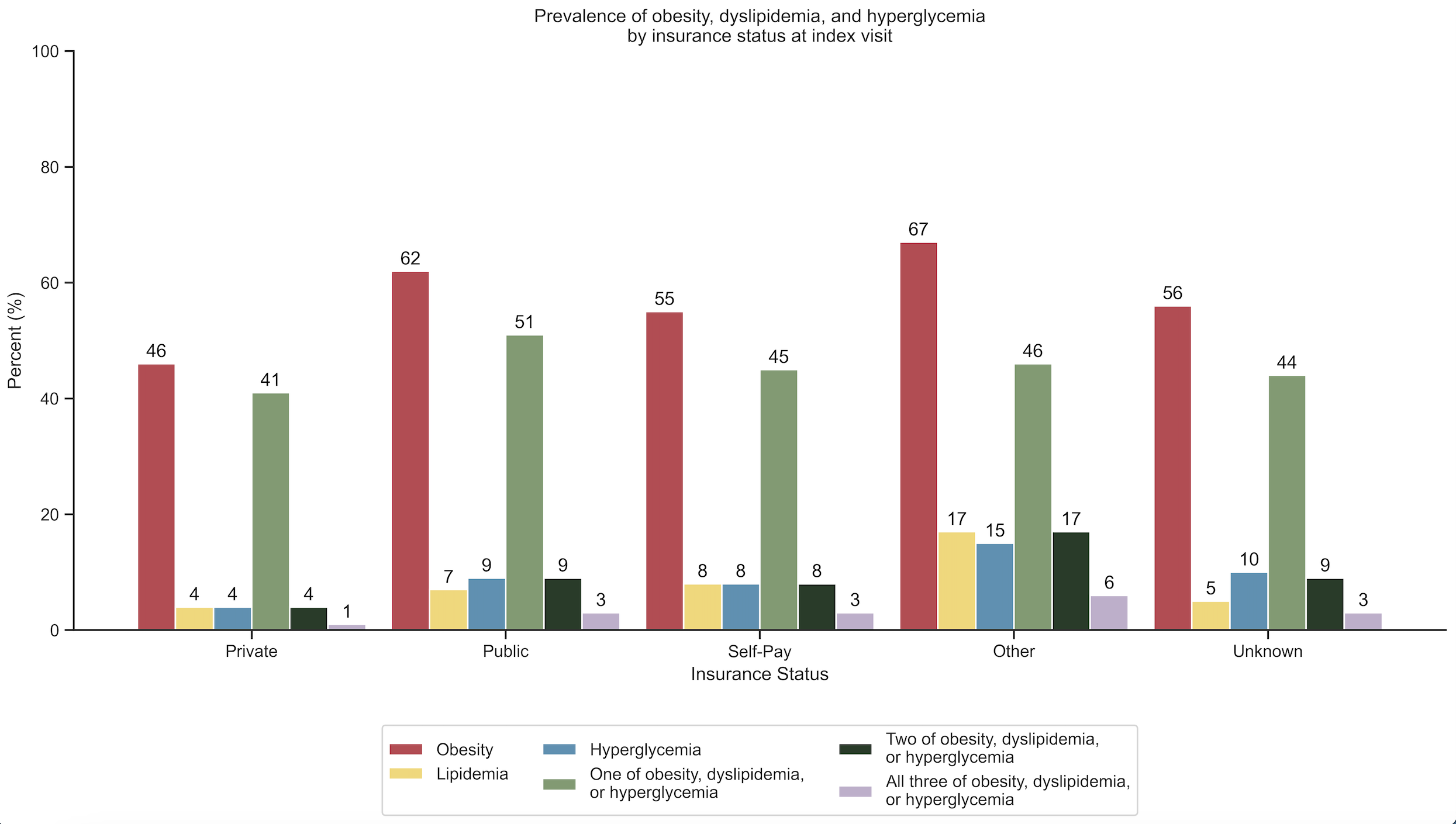
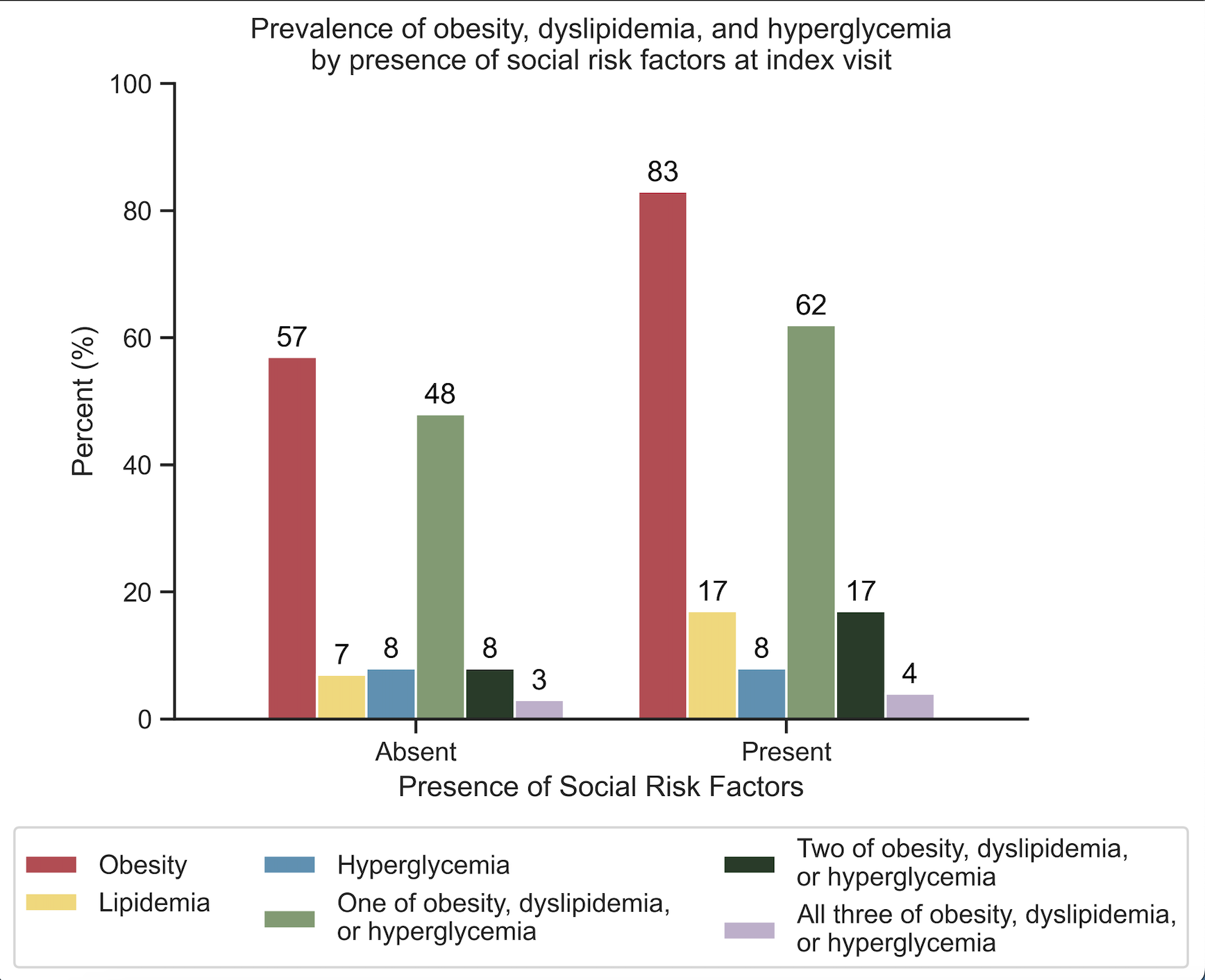
Results: Of the 10,968 participants, mean age was 12.5 years, 38% were female, and 61% had public insurance. On unadjusted analysis, youth with at least one social risk factor had worse CV health factors (OR 2.64, 95% CL 1.59 to 4.39), particularly a 42% elevated risk of obesity and 154% higher risk of dyslipidemia. Youth with public insurance also showed worse overall CV health (OR 1.91, 95% CL 1.76 to 2.08) and greater risks of obesity, dyslipidemia, and hyperglycemia individually. No association was found with BP severity, and youth with public insurance had a lower risk of TOI.
Conclusion(s): In a large multisite cohort of youth referred for HTN disorders, we found that social risk factors were associated with heightened CV risk, specifically obesity and dyslipidemia. Public insurance was also associated with more CV health risk factors but lower risk of TOI. These findings suggest that youth with HTN disorders who experience social risk factors may be at greater risk of developing adverse CV health. Ongoing work will investigate causes of healthcare disparities to inform future management of youth with HTN disorders.