Clinical Bioethics
Session: Clinical Bioethics
426 - Delivery Room Interventions Beyond Intubation for Extremely Early Newborns: Considerations for Counseling
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 426
Publication Number: 426.2090
Publication Number: 426.2090
Isaiah Brown, BS (he/him/his)
Medical Student
University of Chicago Division of the Biological Sciences The Pritzker School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background: Through shared decision-making, physicians and parents make delivery room (DR) care plans for extremely premature newborns who face high risks of neurodevelopmental impairment and death. While intubation is usually the first step of active treatment, the roles of chest compressions (CC) and epinephrine (EPI) require consideration.
Objective: To understand outcomes of extremely early newborns receiving DR interventions beyond intubation
Design/Methods: A retrospective cohort study of birthing persons (BPs) and their newborns delivered between 22+0/7 and 24+6/7 weeks gestation at 13 US training centers in the INDEED study group from 2011 to 2020. Liveborn newborns successfully intubated for attempted resuscitation in the DR were included. We collected sociodemographic and clinical data from medical records of BPs and newborns and extracted census-related American Community Survey data using BPs’ home zip codes. We compared characteristics of newborns who died vs. survived in the DR using Chi test and odds ratios and 95% confidence intervals (OR, CI) for categorical and Student's t-test for continuous variables. Odds ratios for dying before NICU discharge were also calculated.
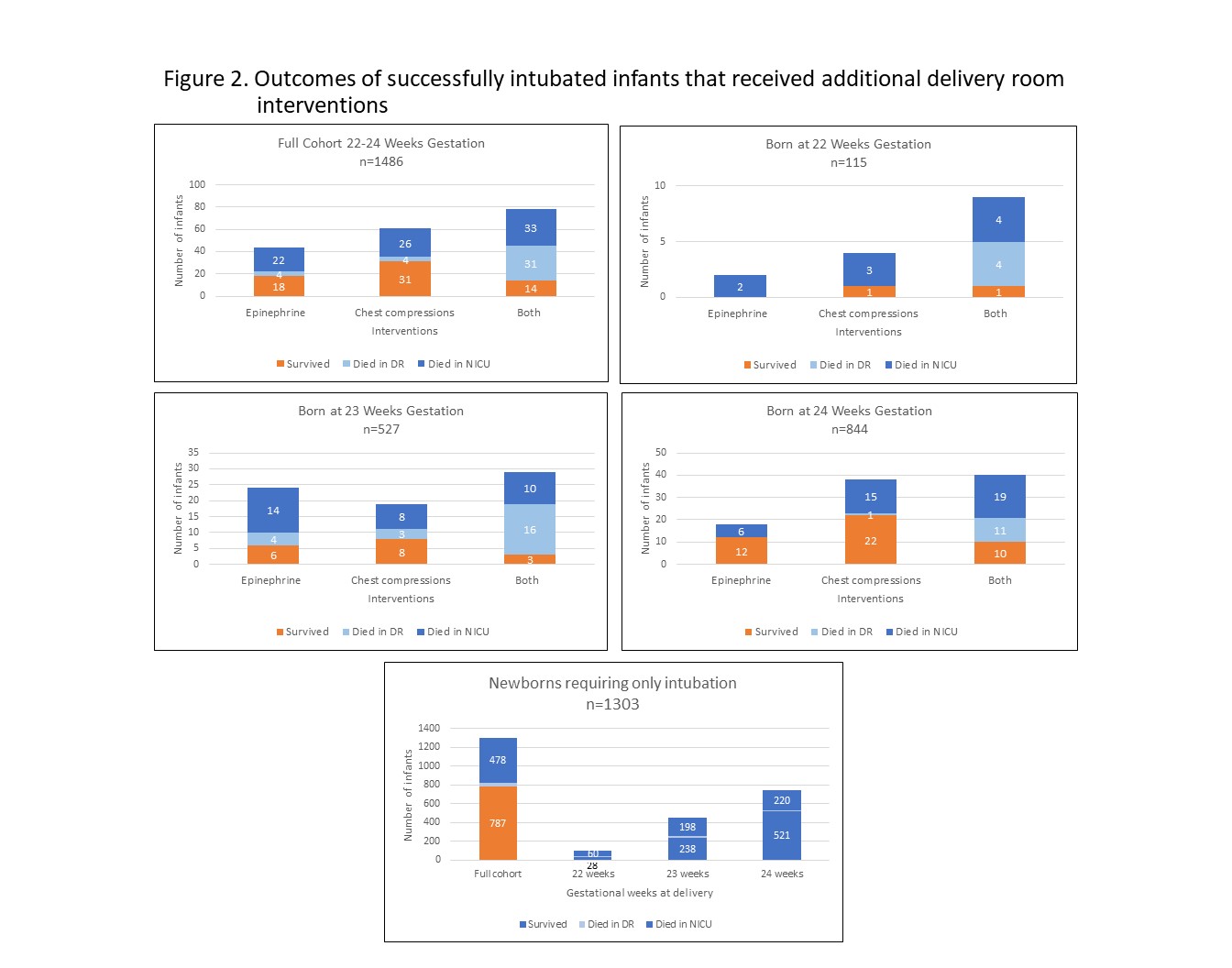
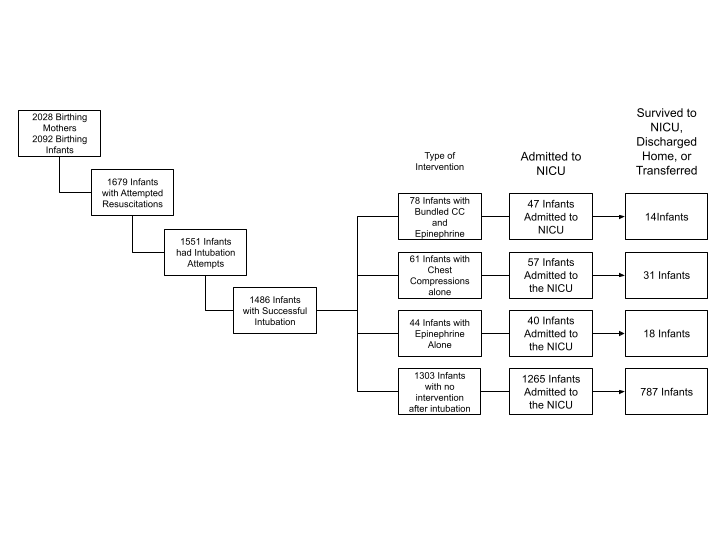
Results: 1486 newborns were included (Figure 1). Table 1 compares those who died vs. survived in the DR. DR death was more likely for those receiving EPI alone (OR 3.33, CI 1.13-9.78, p< 0.045) and CC/EPI bundle (OR 22.0, CI 12.6-38.3, p< 0.001), but not CC alone. Those dying in the DR delivered at lower birth weights and gestational ages. DR death was 4.97 times (CI 1.21-20.5, p=0.014) more likely after delivery for gestational issues (e.g., preterm labor or cervical insufficiency) vs. maternal or fetal concerns. DR deaths did not differ by BPs’ clinical or sociodemographic factors or geocoding data. Figure 2 reports mortality by gestational age. For those admitted to the NICU, odds of death before discharge were higher after DR EPI (OR 2.00, 1.07-3.78, p=0.032) and both EPI/CC bundle (OR 3.87, 2.05-7.30, p< 0.001) but not CC alone (OR 1.38, 0.807-2.35, p=0.265). Overall, odds of death before NICU discharge, regardless of location, were 1.48 times higher after DR EPI (CI 0.883-2.47, p=0.143) and 6.97 times higher after EPI/CC bundle (CI 3.87-12.6, p< 0.001), but not higher after CC alone.
Conclusion(s): Antenatal counseling for parents facing extremely early delivery requires evaluation of risks and benefits. The higher rates of DR and NICU deaths for those requiring more than intubation may inform counseling regarding trials of therapy.