Neonatology
Session: Neonatal Infectious Diseases/Immunology 2
614 - Umbilical cord blood culture positivity in preterm and term neonates: prospective cohort study
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 614
Publication Number: 614.464
Publication Number: 614.464
- AK
Ashutosh Kapoor, MBBS MD DM (he/him/his)
ALL INDIA INSTITUTE OF MEDICAL SCIENCES NEW DELHI
lucknow, Uttar Pradesh, India
Presenting Author(s)
Background: There is a dearth of literature for umbilical cord blood (UCB) culture positivity as a marker of intra-amniotic infection, and its association with prematurity. Further, association with maternal-perinatal risk factors for early onset neonatal sepsis needs exploration.
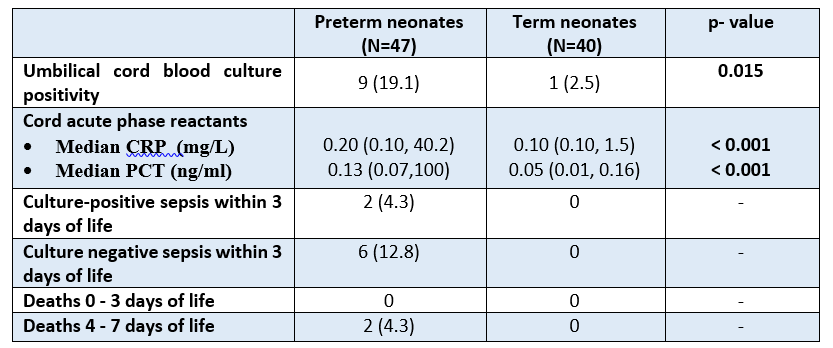
Objective: To compare cord blood culture positivity in preterm neonates ( < 35 weeks) born spontaneously and term neonates (37-41 weeks). The secondary objectives were to compare cord blood culture positivity in three subgroups of preterm neonates based on their exposure to risk factors for sepsis and intrapartum antibiotics.
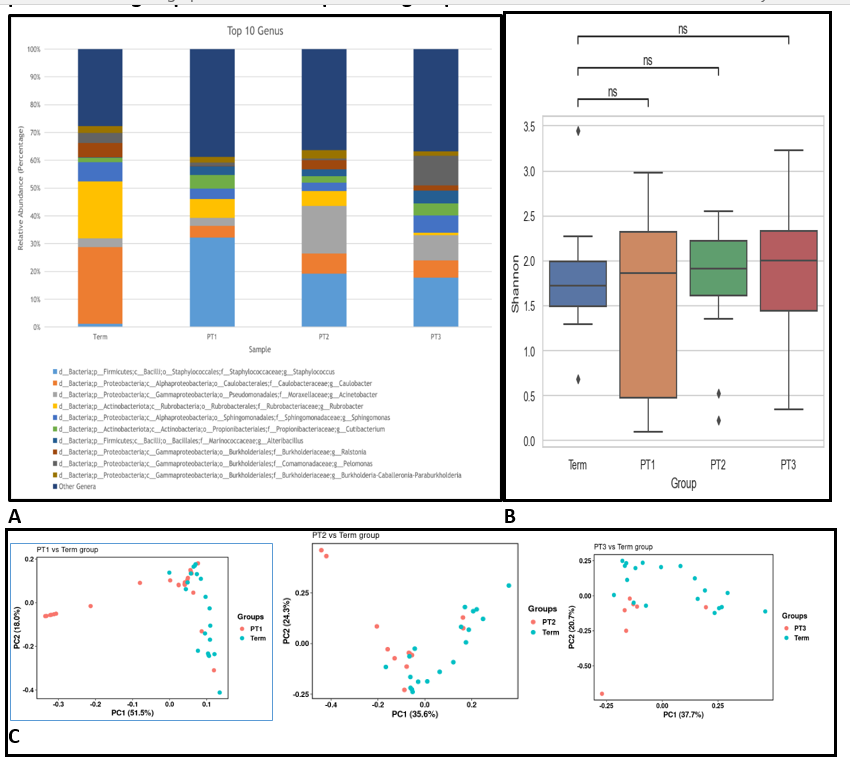
Design/Methods: Umbilical cord blood was collected from both the sides of the umbilical cord using a standardized protocol, from mothers with spontaneous onset of preterm labor and those with term gestation (unexposed to antibiotics with no risk factors for sepsis) post-delivery from June 2021 to May 2022 at a tertiary unit in India. We performed bacterial culture using automated bactec system, measured acute phase reactants in serum and sequenced the sample for 16S rRNA. Neonatal blood sample within 2 hours of birth was also collected. Neonates were followed for the first 72 hours for clinical signs of sepsis and any death was recorded until seven days of life.
Results: We enrolled 40 mothers each (47 preterm and 40 term neonates) in term and preterm groups. Cord blood culture positivity was significantly higher in preterm group 19.1% (9/47) as compared to term group 2.5% (1/40) (RR 7.6; 95% CI 1.0-57.9; p=0.015). The organisms isolated in the preterm group from UCB samples were Escherichia coli (n=4), Enterococcus faecium (n=1), Staphylococcus hominis (n=2), Staphylococcus epidermidis (n=1), Lysinibacillus fusiformis (n=1). The only isolate in term group was Acinetobacter baumannii (n=1). All the 9 UCB culture positive in the preterm group had additional risk factors at birth for sepsis and were exposed to intrapartum antibiotics. Among these 9 neonates with UCB culture positive results, 6 developed sepsis (2 culture-positive sepsis and 4 clinical sepsis) as compared to 2 clinical sepsis among 38 UCB culture-negative. Escherichia coli was the pathogen in both the culture-positive neonates, which was in concordance with the UCB culture results. Antibiotic sensitivity pattern of E coli was also concordant in both the cases. Whole genome sequencing was done for one set of E coli from UCB and neonatal blood, and it was found to be the same sequence type (ST11).
Conclusion(s): Umbilical cord blood of spontaneously delivered preterm neonates with maternal risk factors exhibit a higher rate of culture positivity.
.png)