Neonatology
Session: Neonatal Follow-up 4
552 - Neurodevelopmental outcomes and multimorbidity after IVH grade 1-2: a population matched cohort study of extremely preterm infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 552
Publication Number: 552.2917
Publication Number: 552.2917

Philippa Rees, BSc (Hons) MPhil MBBCh MRCPCH
NIHR Doctoral Fellow
UCL Institute of Child Health
London, England, United Kingdom
Presenting Author(s)
Background: Prematurity and its sequelae are a major cause of childhood morbidity. Low-grade IVH was previously reported to have little long-term impact although evidence is now conflicting.
Objective: To undertake a population cohort study of infants born at < 29 weeks’ gestation in England between 2013-2019 to determine incidence of low-grade IVH and neurodevelopmental outcomes.
Design/Methods: All preterm infants < 29 weeks’ gestation diagnosed with IVH grade 1-2 on imaging, and their 1:1 propensity score matched controls without brain injury were included from the National Neonatal Research Database (NNRD). The NNRD includes data for all UK infants admitted to a neonatal unit. The national incidence of low-grade IVH was calculated. Infant characteristics were explored including the presence of morbidities such as culture-positive sepsis, receipt of major surgery, necrotising enterocolitis, retinopathy of prematurity and bronchopulmonary dysplasia. The primary outcome was normal developmental at 2 years’ corrected age; secondary outcomes were severity of developmental delay; and functional impairment in communication, motor, visual, and auditory function. Inverse probability weighting was used to account for missing data. Crude and adjusted risks were determined in multivariate logistic regression models.
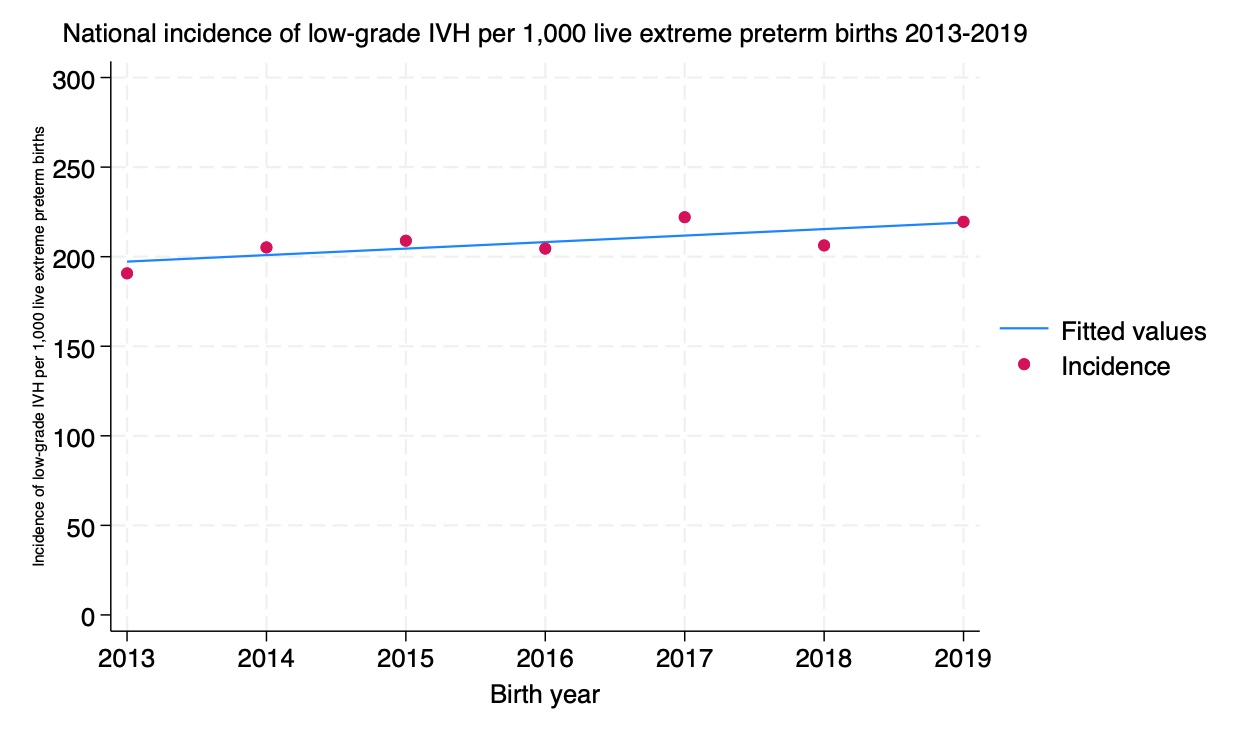
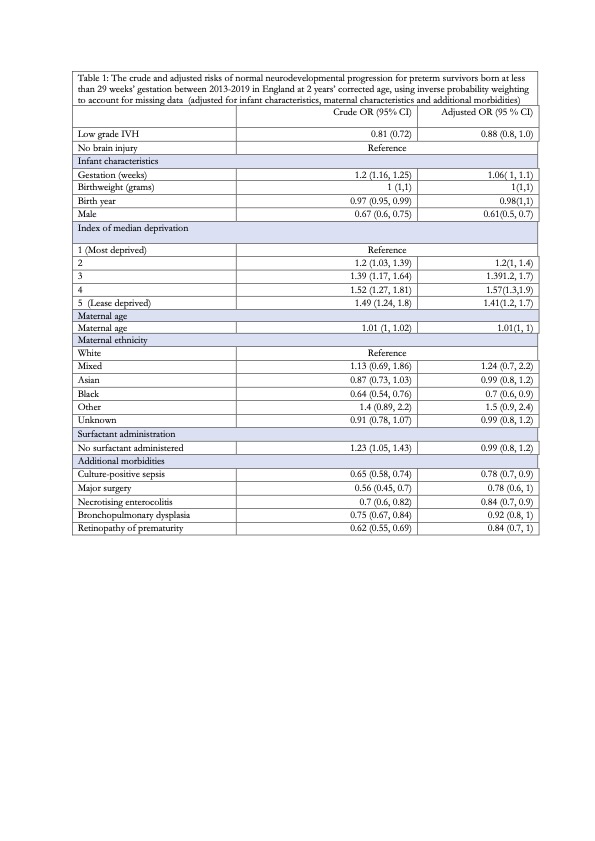
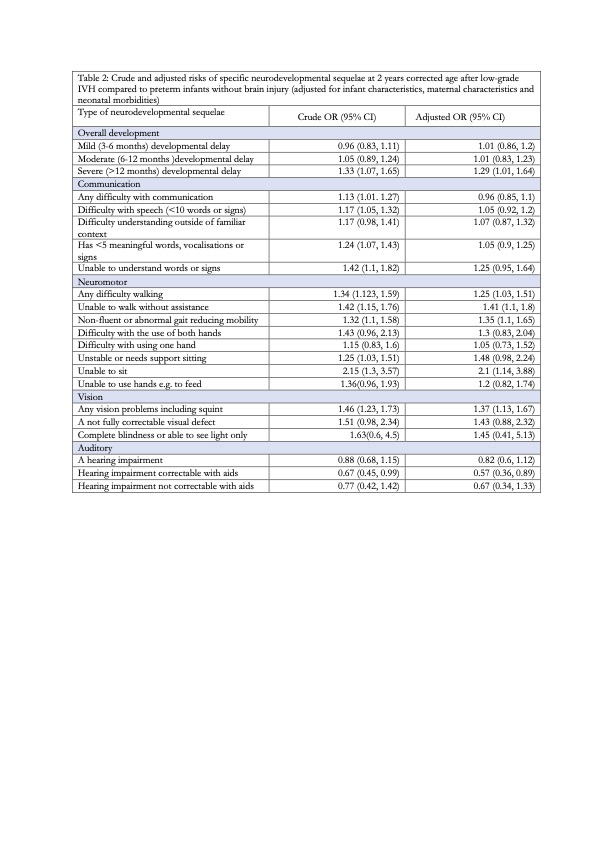
Results: This study included 11140 infants, of which 5570 had low-grade IVH, 2743 grade 1 and 2827 grade 2. The national incidence of low-grade IVH amongst extreme preterm infants was 20.8%. Low-grade IVH incidence increased between 2013-2019 (r= 3.66 95%CI (-0.2, 7.3; Figure 1). More infants with low-grade IVH had multi-morbidities (n=4390,78.8%) than controls (n=3261, 58.5%). Follow-up data were available for 79% of survivors. Most surviving infants with low-grade IVH (n=1773, 57.9%) were developmentally normal at 2 years, this was slightly higher for controls (n=1571, 62.9%). The likelihood of normal development was lower after low-grade IVH OR 0.81 95%CI( 0.73 0.91), but much of this association was attenuated on adjusting for multi-morbidities aOR 0.88 95%CI (0.78, 1.0) (Table 1). The absolute risk of moderate-severe delay were low after low-grade IVH (19.4%) and for controls (16.6%). Of those low-grade IVH who did experience developmental impairment, functional motor and visual impairments predominated (Table 2).
Conclusion(s): This population study reports that although one in five extreme preterm infants have a low-grade IVH many are developmentally normal. These positive findings should inform prognostic discussions with parents, although population studies of later childhood outcomes are required.