Neonatology
Session: Neonatal Quality Improvement 4
65 - Optimizing Oxygen Saturation Targeting for Preterm Infants: Significant Increase in Time in Target Range and the Effect on Retinopathy of Prematurity
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 65
Publication Number: 65.2916
Publication Number: 65.2916

Sanoj KM Ali, MD FRACP
Attending Physician
Sidra Medicine
Doha, Ar Rayyan, Qatar
Presenting Author(s)
Background: The controversial history of oxygen use in preterm infants and recent systematic reviews have shown that liberal oxygen administration is associated with retinopathy of prematurity (ROP) and bronchopulmonary dysplasia (BPD), whereas restrictive use results in increased mortality and neurodisability. The current standard of care for continuous assessment of oxygen saturation levels (SpO2) is pulse oximetry. Observational studies in NICU have shown that SpO2 levels in preterm infants are maintained within the prescribed target range (TR) only a third to 50% of the time.
The rate of retinal detachments and severe ROP was unacceptably high following the activation of our quaternary NICU services in 2018. This was a “greenfield” NICU, integrating heterogeneous practices within a highly skilled, but multi-national workforce. Optimization of SpO2 targeting in this preterm population offered the opportunity to bring about significant improvement in their long-term outcome.
Objective: The aim of this quality improvement project (QI) was to increase the time spent within the prescribed SpO2 TR over a three phase ‘plan-do-study-act’ (PDSA) cycle for preterm infants less than 36 weeks gestational age receiving supplemental oxygen via both invasive and non-invasive respiratory support.
Design/Methods: A prospective audit was undertaken to collect information regarding baseline staff knowledge of alarm limits, SpO2 targets and evaluation of time spent BELOW, IN and ABOVE TR, which was used to guide the initial phase of the PDSA cycle.
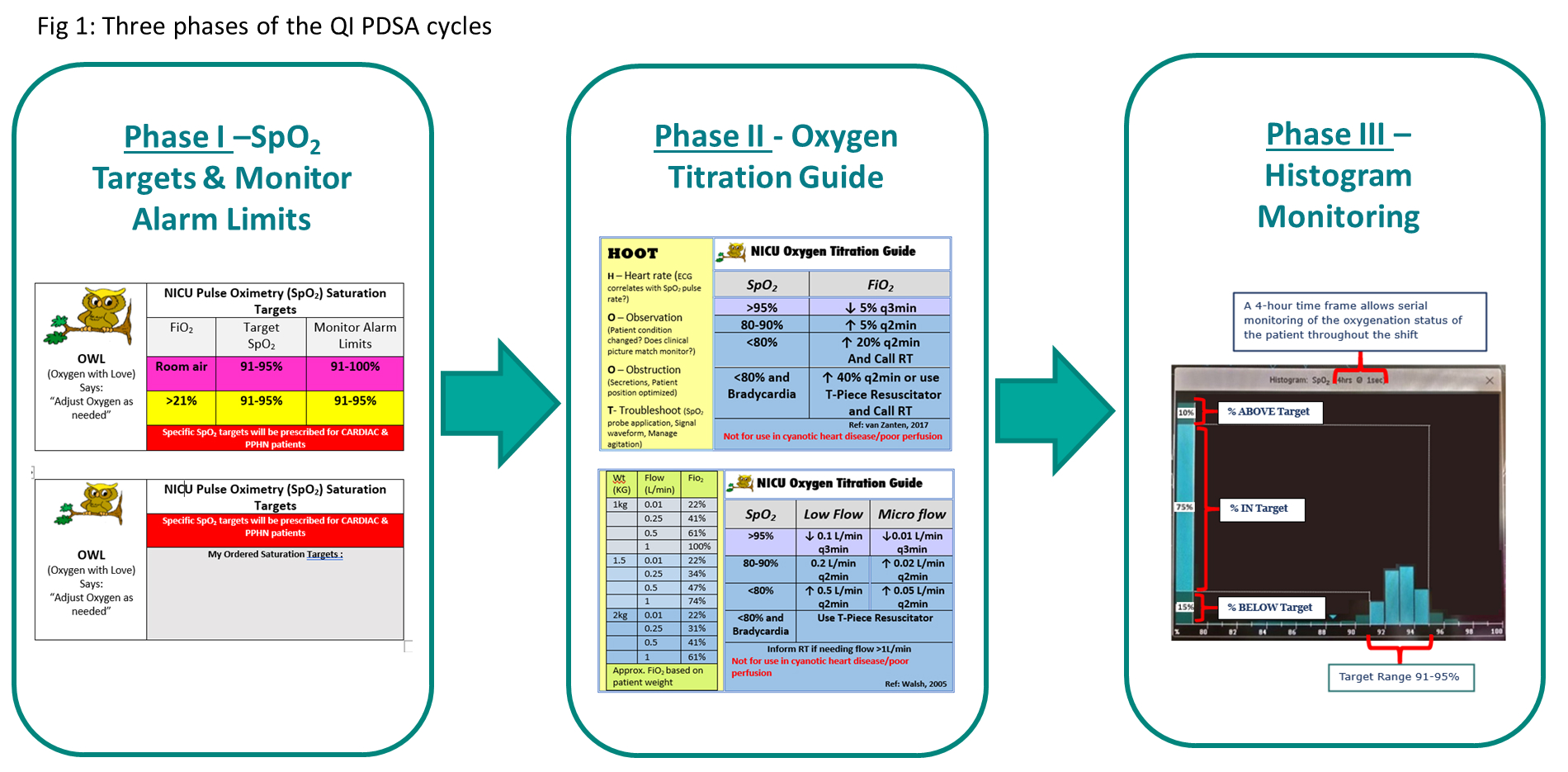
Phase 1 –Standardization of SpO2 TR (individualized TR for those with congenital cardiac anomalies) and bedside monitor alarm limits.
Phase II – Introduction of a structured oxygen titration guide.
Phase III – Implementation of bedside histogram monitoring and inclusion in multidisciplinary ward round discussion (Fig 1).
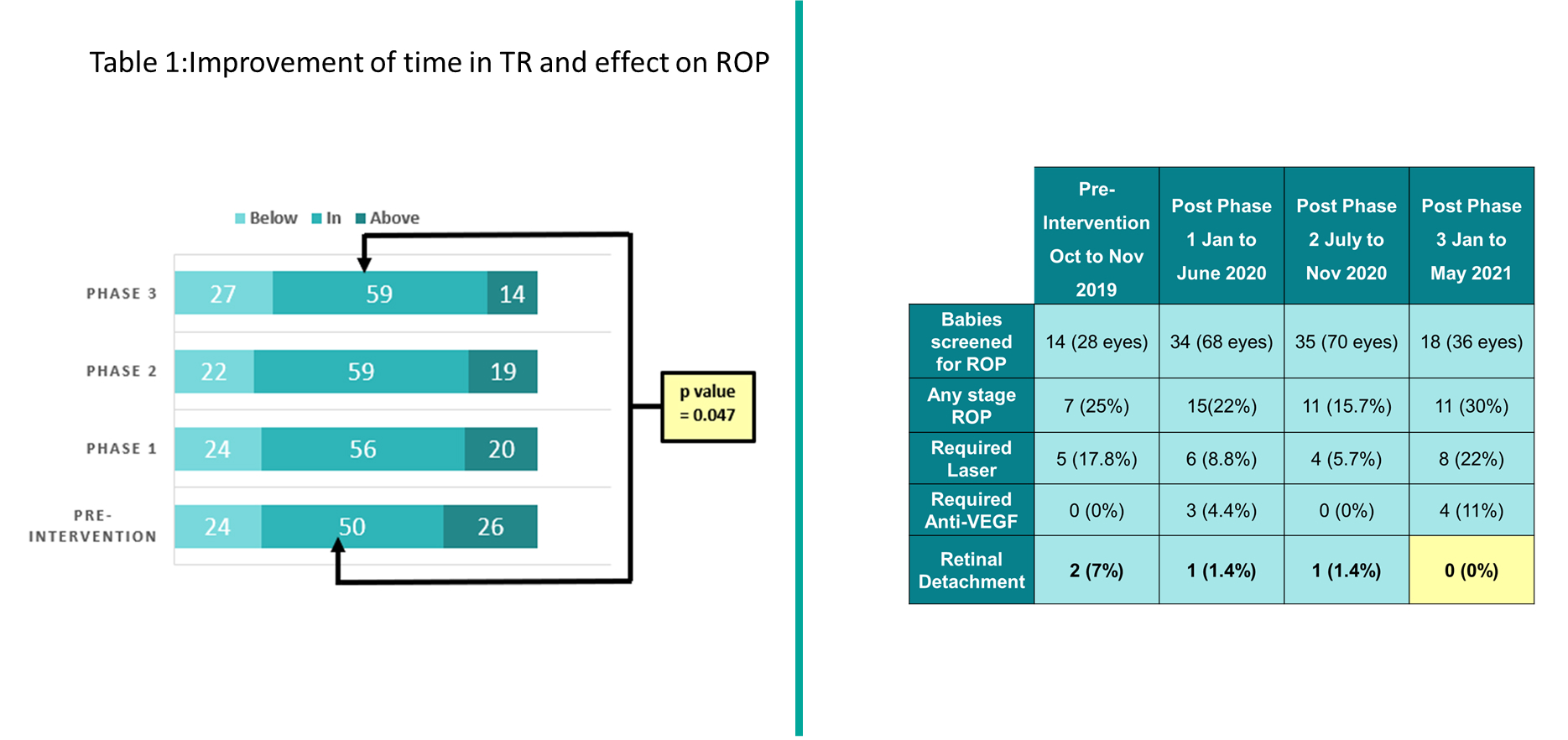
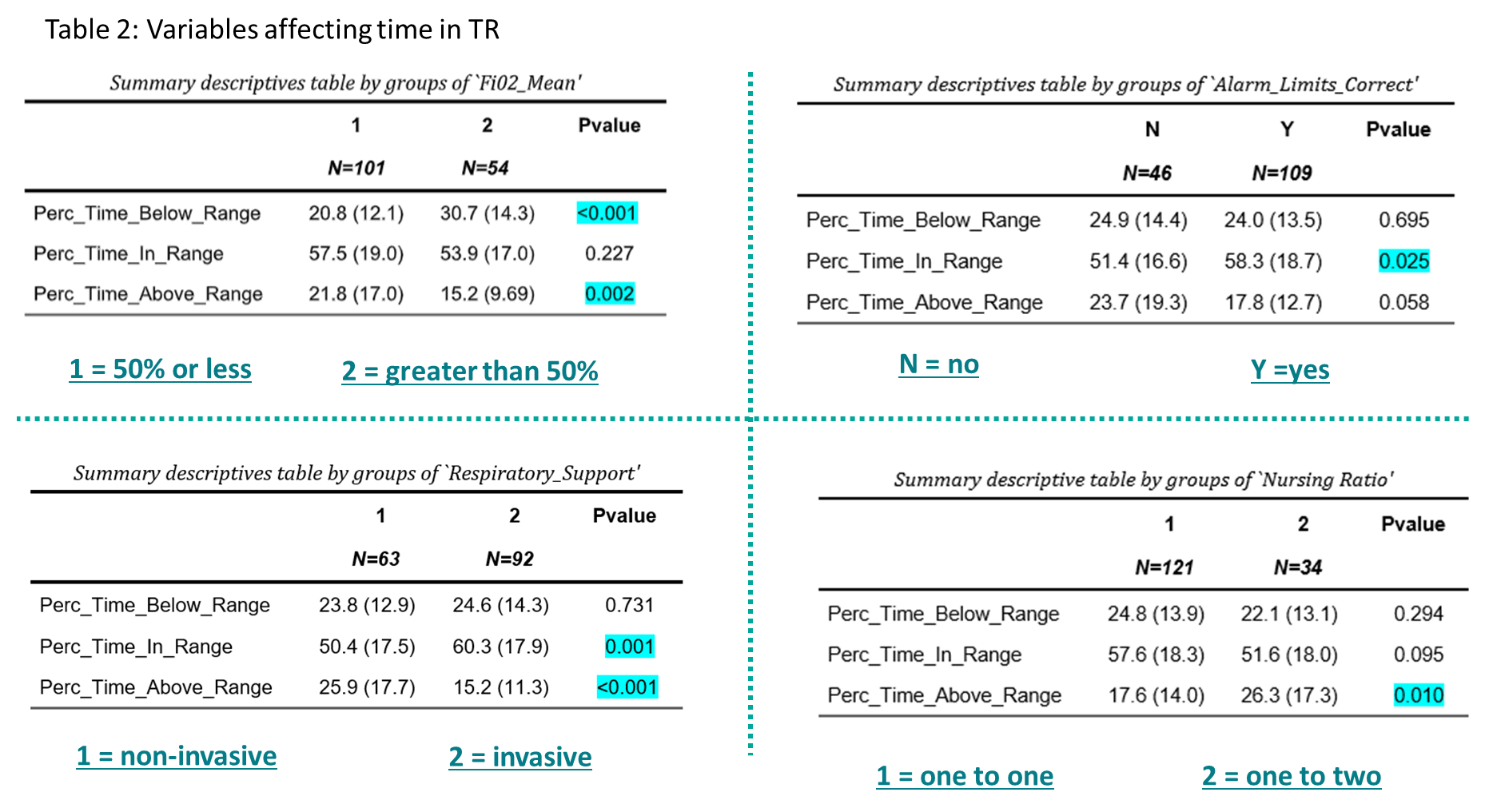
Results: Post phase I, the appropriate setting of bedside monitor alarm limits increased from 12 to 100%. Following the phase II intervention implementation, the rate of any stage ROP decreased from 25 to 15.7%. After phase III, there was a significant increase in time spent IN target range from the pre-intervention baseline (p=0.047) and there were no retinal detachments over a two year follow up period (Table 1). Improved SpO2 targeting was also noted in infants on invasive respiratory support, when nursed 1:1 and in those who had the correct alarm limits set on the bedside monitors (Table 2).
Conclusion(s): This three phased PDSA QI project improved the time spent in TR as well as reduced the incidence of retinal detachment in our NICU.