Neonatology
Session: Neo-Perinatal Health Care Delivery 1: Epidemiology/Health Services Research
316 - Elusive Optimum Oxygen Saturation Targets Despite 5 Randomized Clinical Trials and Meta-analysis of 4,965 infants – Do We Have an Answer?
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 316
Publication Number: 316.1237
Publication Number: 316.1237
- MH
Mahira F. Hassan, BSc in Progress (she/her/hers)
Student
University of Calgary, Cumming School of Medicine
Edmonton, Alberta, Canada
Presenting Author(s)
Background: Despite 5 Randomized Clinical Trials, a systematic review (Manja et al, 2017) and NeOProM meta-analysis comprising 4,965 infants (Aski et al, 2018), optimum SpO2 targets remain elusive. In view of the higher infant mortality rates associated with lower SpO2 targets and intermittent hypoxemic episodes, Europ. Consensus guidelines (Sweet et al, 2019) and American Academy of Pediatrics (2016) recommended the SpO2 targets of 90-94% in infants born ≤28 wk postmenstrual age (PMA). Since then, several neonatal centers including ours increased the SpO2 targets from 88-92% to 90-95%.
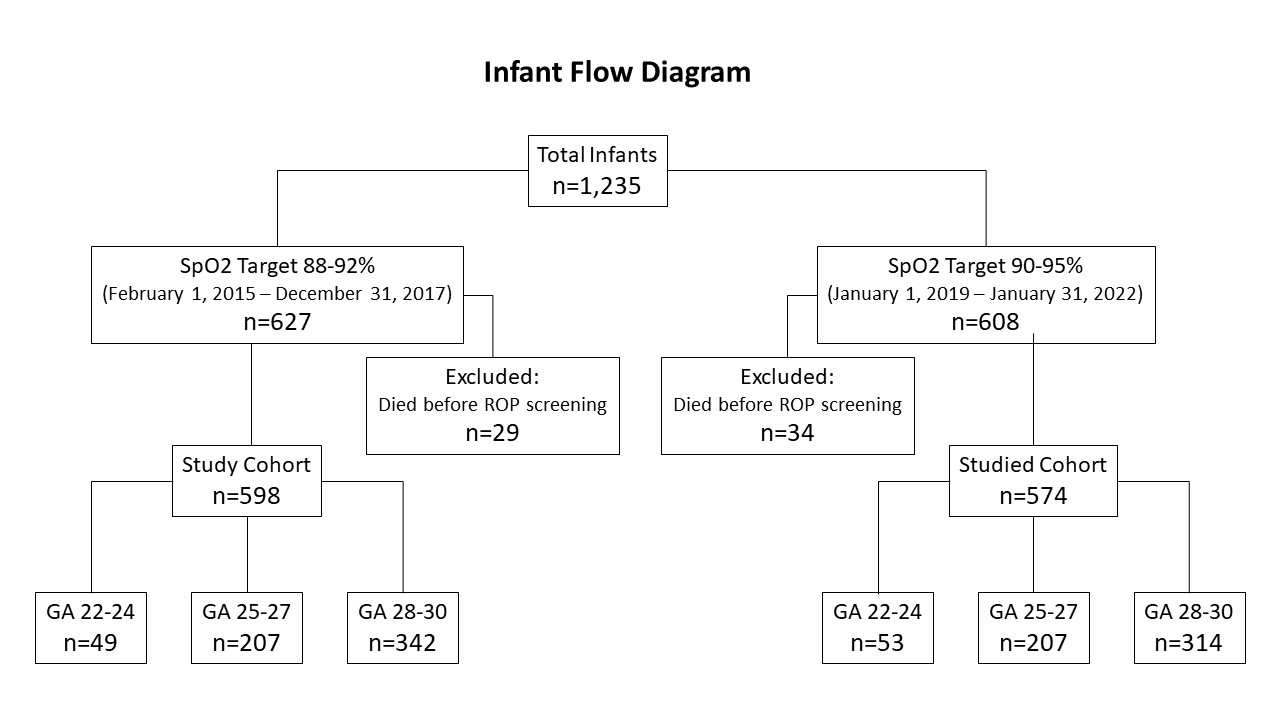
Objective: To investigate the impact of increased SpO2 targets from 88-92% to 90-95% on mortality and morbidities in 1,235 infants born between 22-30 weeks PMA at a large tertiary care Canadian perinatal center.
Design/Methods: Our study comprised of a retrospective (SpO2 targets 88-92%; 2015-2017, n=627) and a prospective (SpO2 targets 90-95%; n=608, 2019-2022) cohort of infants born between 22-30 weeks PMA. The primary outcome was the occurrence and severity of retinopathy of prematurity (ROP). Secondary outcomes included death prior to discharge home, bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL) and sepsis. The data were stratified into 22-24, 25-27 and 28-30 weeks PMA (Figure 1). Maternal and infant characteristics and variables are given in Tables 1 and 2, respectively. All continuous variables were compared using Kruskal Wallis test and all categorical variables were compared using Chi-sq test (SAS v 9.4).
Results: The incidence of ROP, its severity and number of treatments increased in the higher SpO2 cohort (p=0.02 - < 0.001). BPD rates increased from 44.7% to 52.8% (p=0.004). Higher number of babies received high frequency ventilation (p < 0.001), exposure to O2 (p=0.01), increased mild-moderate IVH (p < 0.005), PVL (p < 0.0001), surgical NEC (p=0.03) and home O2 therapy (p < 0.05). The mortality, sepsis or PDA ligation rates, length of hospital stay, and home gavage feeds were similar between the two groups. Higher morbidities were not attributable to birth weight, sex, outborn status, SGA, antenatal glucocorticoid use, SNAP/SNAP-PE, Apgar scores, umbilical cord pH or duration of parenteral nutrition.
Conclusion(s): SpO2 targets of either 88-92 or 90-94% should not be instituted uniformly. In perinatal centers with low baseline mortality, NEC, IVH and ROP rates, and high BPD rates, raising the SpO2 targets from 88-92% to 90-95% are not recommended as they may lead to adverse effects on morbidities without decreasing mortality rates
.jpg)
.jpg)
