Child Abuse & Neglect
Session: Child Abuse & Neglect 2
183 - Diagnostic Error in the Evaluation of Abusive Head Trauma
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 183
Publication Number: 183.1211
Publication Number: 183.1211

Lindsey S. Herberger (she/her/hers)
Medical Student
University of Arkansas for Medical Sciences College of Medicine
Little Rock, Arkansas, United States
Presenting Author(s)
Background: A 1999 study of abusive head trauma (AHT) identified that >30% of cases of AHT were missed, and more frequently so in young infants, white families, and two-parent homes. Since that time, factors associated with diagnostic error may have changed.
Objective: We aim to identify current rates of and characteristics associated with diagnostic error in AHT.
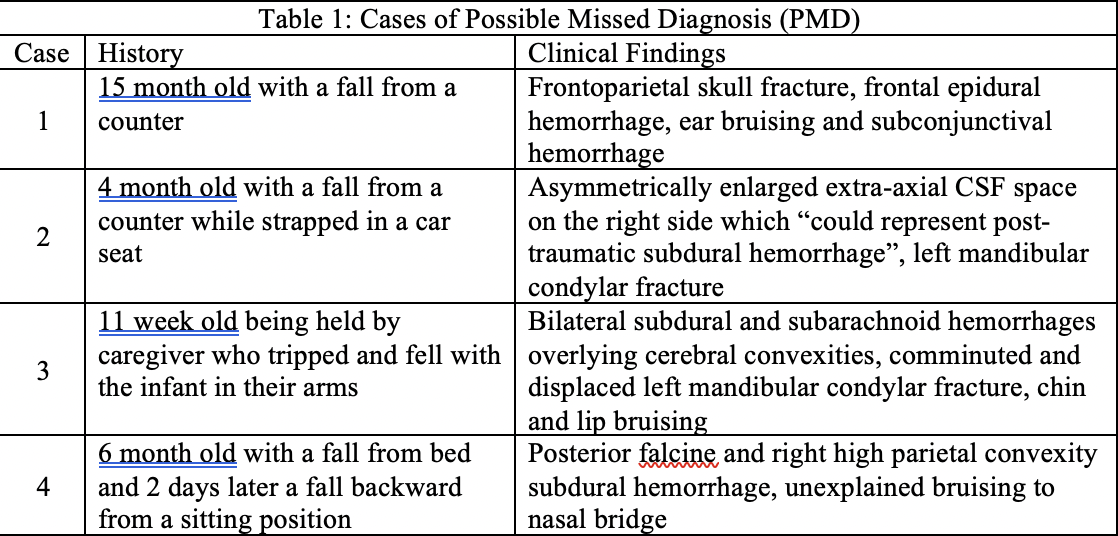
Design/Methods: This is a single institution, case-control retrospective review of patients < 3 years with an intracranial injury suspicious for AHT. Patients with a diagnostic code for head injury and a skeletal survey between Jan ’15-May ’23 were manually reviewed for inclusion. AHT was defined as a documented diagnosis by a board-certified Child Abuse Pediatrician. Diagnostic errors were defined as 1) Missed Diagnosis (MD); a patient seen for symptoms compatible with head trauma, discharged home, returning with a diagnosis of AHT 2) Delayed Diagnosis (DD); a patient not receiving an initial evaluation for AHT but admitted and diagnosed with AHT during their hospitalization and 3) Possible Missed Diagnosis (PMD); a patient with suspicious injuries not receiving an evaluation for AHT. We completed our analysis with and without PMD cases included due to inability to confirm a diagnosis. Investigators recorded demographics, clinical presentation, presence of high-risk bruising defined by the TEN-4-FACESp clinical decision rule and diagnostic error. Statistical analysis included descriptive statistics and chi-squared tests.
Results: 118 cases of AHT were identified, including 107 (90.7%) without diagnostic error and 11 (9.3%) with MD/DD. There were no significant relationships between demographics/social factors and MD/DD, but this may be due to insufficient power. High-risk bruising was identified in 4/11 (36.4%) cases of MD/DD. There were 4 cases of PMD (Table 1). Including PMD, white children were more likely to have a diagnostic error with 12/15 (92.3%) cases of MD/DD/PMD in white children versus 1/15 (7.7%) black child (p=0.011), and there was an association between a correct diagnosis and presentation with a seizure (p=0.013) or caregiver concern for bruising (p=0.025).
Conclusion(s): AHT is missed at a lower rate than previously identified but race remains a potential contributing factor at our institution. With >30% of missed or delayed diagnoses having high-risk bruising on exam, increased attention to bruising may be an opportunity for improved identification of AHT.