Nephrology
Session: Nephrology 2
19 - Epstein Barr Virus DNAemia in Pediatric Solid Organ Transplant Recipients: A Single Center Study
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 19
Publication Number: 19.1210
Publication Number: 19.1210

Fatema Hammad, MD (she/her/hers)
Pediatric Nephrology Fellow
Children's Hospital of Michigan
Detroit, Michigan, United States
Presenting Author(s)
Background: Pediatric solid organ transplant (SOT) recipients commonly experience Epstein-Barr virus (EBV) DNAemia, posing them at risk of developing post-transplant lymphoproliferative disorder (PTLD). There is scarcity of literature on comparison of risk factors and associated complications of EBV DNAemia in various pediatric SOTs.
Objective: To study the prevalence and risk factors for development of EBV DNAemia and PTLD in pediatric SOT recipients, to compare the clinical presentation, severity, duration and management of EBV DNAemia based on the organ transplanted (kidney, heart, and liver); and finally compare the outcomes of EBV DNAemia with non-EBV DNAemia group.
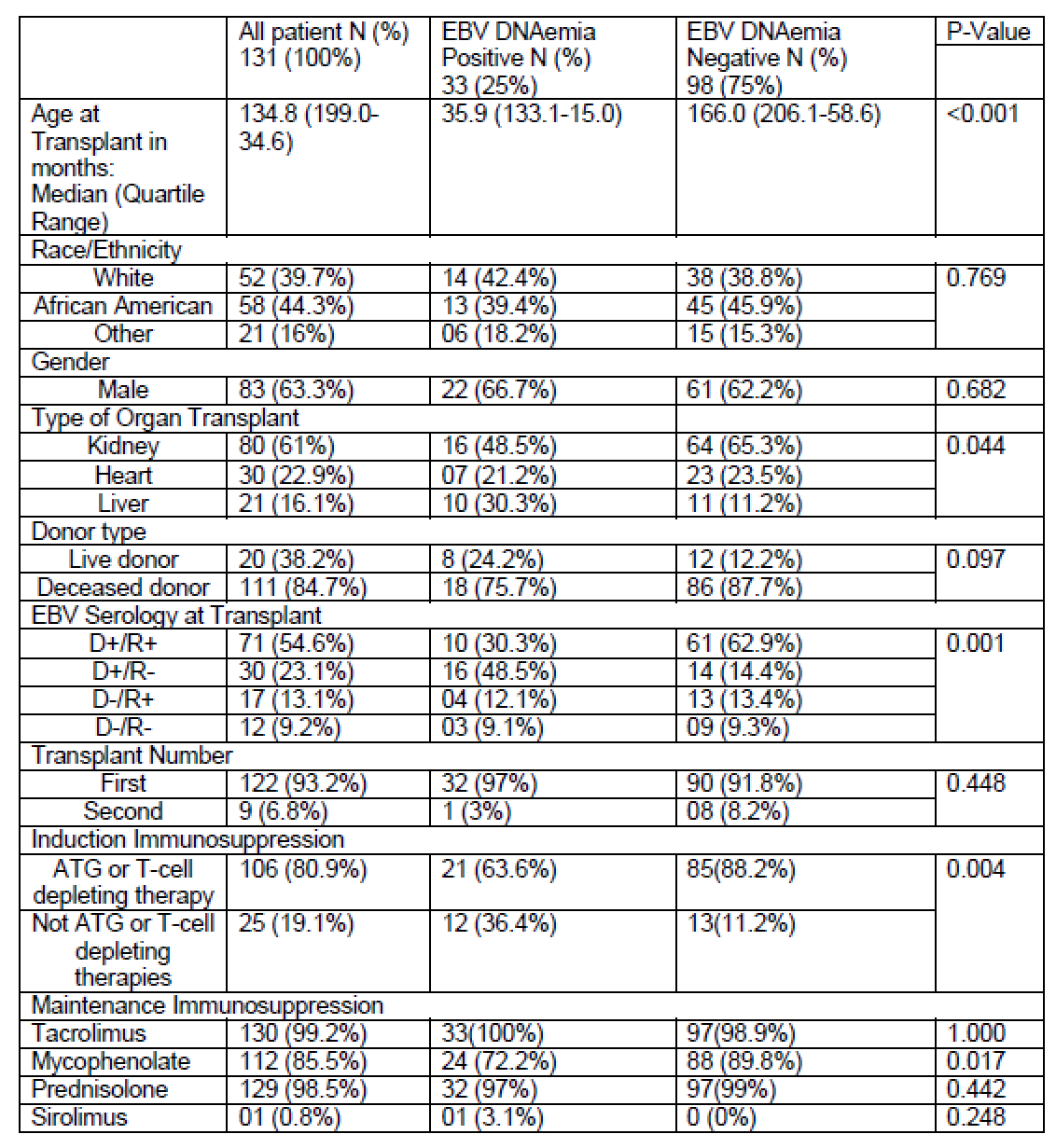
Design/Methods: This retrospective study included children ≤21 years who underwent SOT (kidney, heart, and liver) at a single center between January 1, 2010 and March 31, 2022. Those with incomplete data, and multi-visceral transplant were excluded. EBV DNAemia was defined as ≥ 120 copies/ml of the virus by polymerase chain reaction assay. Wilcoxon test and Pearson’s Chi-squared/ Fisher-Exact test analysis performed using SAS (version 9.4).
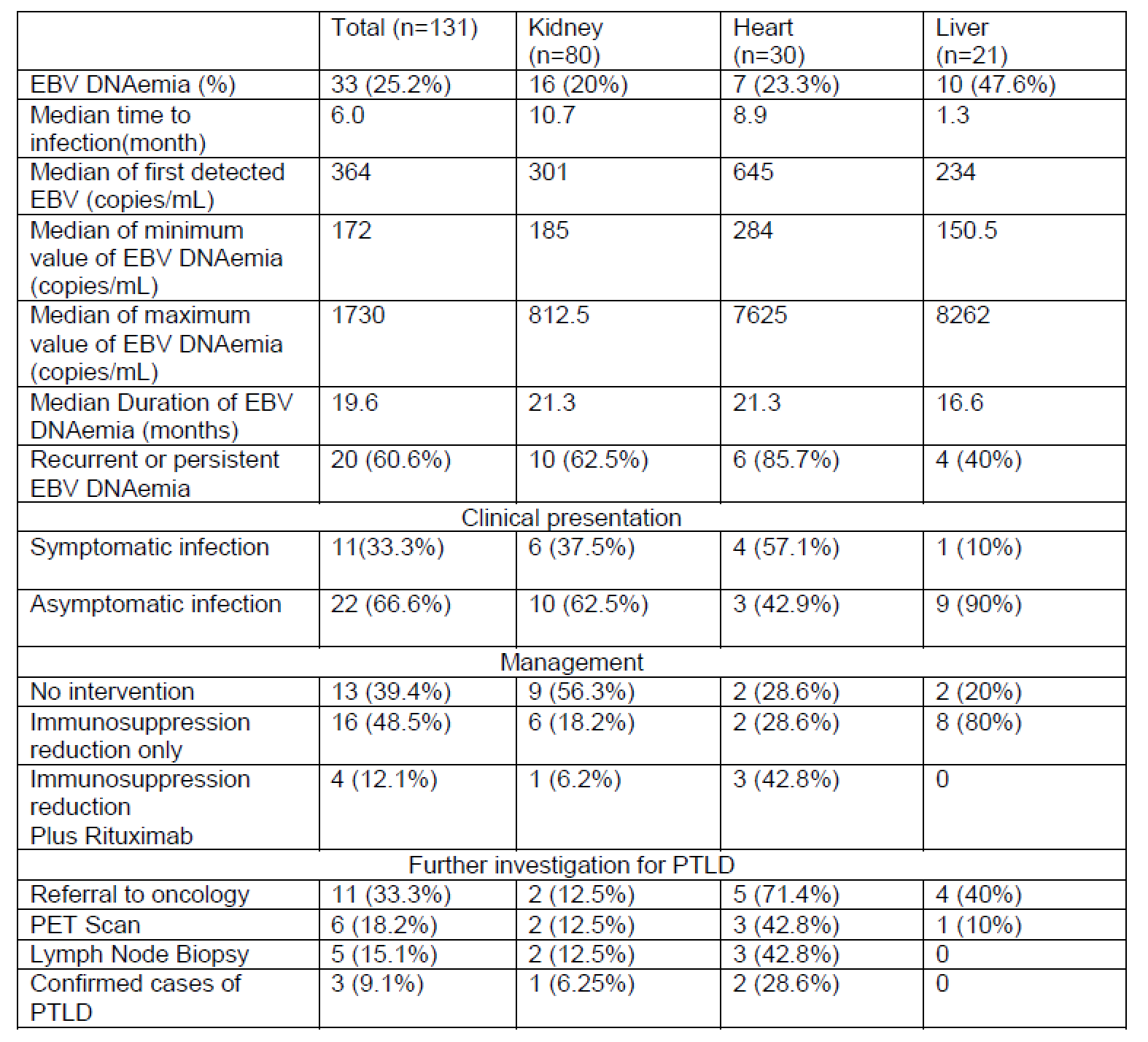
Results: Out of 131 SOT recipients, 33 (25%) had EBV DNAemia. Liver transplant recipients exhibited a higher prevalence of EBV DNAemia (47.6%) among all SOT, followed by heart (23.3%), and kidney (20%) transplant recipients. Significant risk factors for development of EBV DNAemia were type of organ (p=0.044), younger age (p < 0.001), Donor+/Receipent- EBV serology status (p=0.001) and type of induction immunosuppression (p=0.004). Liver recipients had shortest median time to infection (1.3 months) and shortest median duration of infection (16.6 months). Kidney recipients had the lowest median EBV PCR values range (185-812 copies/mL). EBV DNAemia was asymptomatic and detected during surveillance in 66%, recurrent or persistent EBV DNAemia seen in 60.6%; and 48.5% required only reduction in immunosuppression. Oncology consultation was done in one-third of patients with EBV DNAemia, and only 3 patients (9%) developed PTLD compared to 2 (2%) in the non-EBV group. There were no significant differences in other outcomes (rejection episodes, CMV infection, BK infection, and graft loss) between EBV DNAemia vs. non EBV DNAemia group.
Conclusion(s): Organ transplant type (liver>heart>kidney), younger age, donor/recipient EBV serology status, and induction method was strongly associated with development of EBV DNAemia in pediatric SOT recipients. PTLD development was more commonly seen in heart transplant recipients and was not observed in liver recipients despite a higher prevalence of EBV DNAemia.