Medical Education
Session: Medical Education 3
544 - Effectiveness Of A Novel MultiModal Educational Intervention For Improving Shared Decision-Making Skills Among Pediatric Hospitalists
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 544
Publication Number: 544.488
Publication Number: 544.488
.jpg)
Julio D. Ortiz, MD (he/him/his)
Assistant Professor
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Shared decision making (SDM) is a collaborative process where patients, parents and providers work together to make family-centered healthcare decisions. Little is known about how teaching impacts pediatric providers in the inpatient setting.
Objective: We sought to evaluate the effect of a novel multimodal educational intervention on Pediatric Hospital Medicine (PHM) faculty’s skills, knowledge, attitudes and self-reported behaviors toward SDM.
Design/Methods: We conducted a prospective single center study from 7/2021- 1/2023 of PHM attending physicians at our institution. Faculty participated in three educational interventions from 2/2022 to 4/2022: an asynchronous online module, a one-hour didactic lecture on patient decision aids (PDAs), and a 2-hour interactive workshop. Additionally, PDAs were developed as tools for practice. Outcomes were measured pre- and post-intervention for comparison. The primary outcome was faculty SDM skills in a simulated encounter with a standardized patient scored by trained, blinded scorers using the validated OPTION 5 scale. Secondary outcomes included: knowledge, attitudes towards SDM, self-reported behaviors and decision-style. Paired analyses were conducted using Wilcoxon matched-pairs signed rank test and McNemar’s chi-squared exact method to evaluate for statistically significant differences (p < 0.05) in pre- vs. post-intervention period
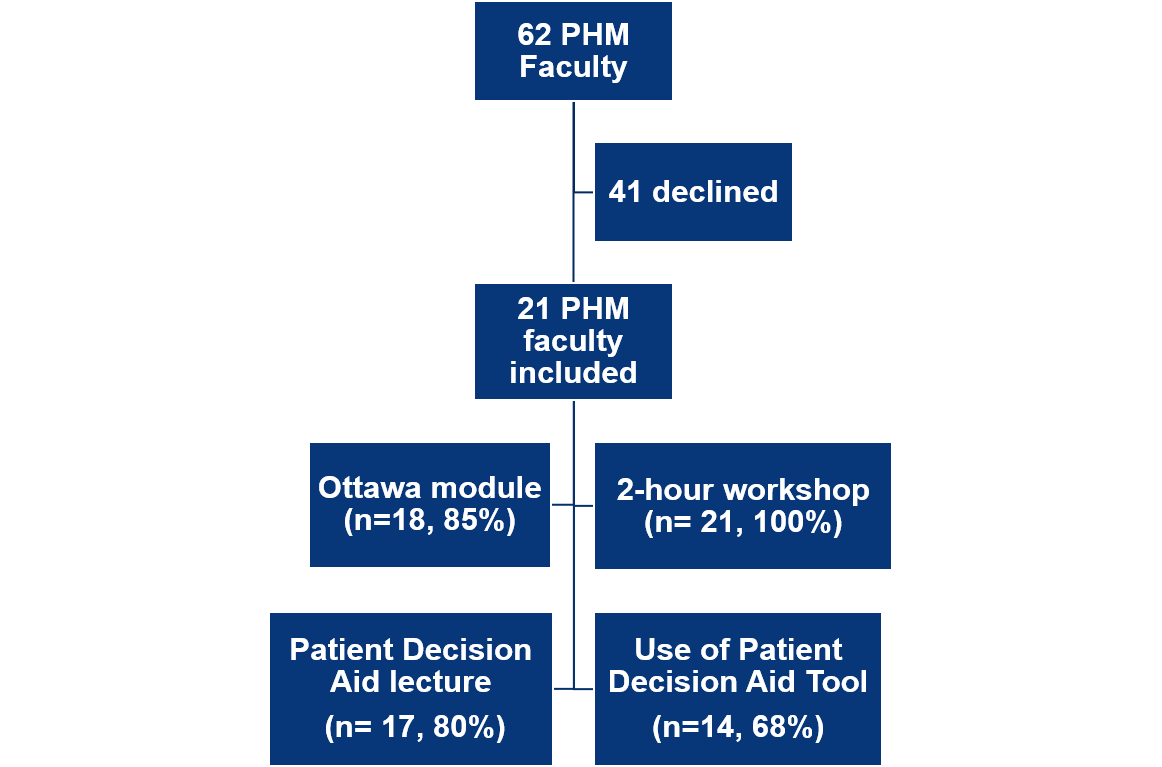
Results: Of the 62 faculty approached, 21 PHM faculty participated in the study. Faculty were a median 7 years (range 3-34 years) post-residency training and 19 faculty (90%) had no previous SDM training.. Faculty participation was highest for the workshop (100%), then the Ottawa module (85%) and PDA lecture (80%). Faculty SDM skills in a simulated encounter improved post-interventions with a median pre-score of 37.5 (IQR 35.0, 42.5) and post-score of 45.0 (IQR 40, 52.5), p= 0.02. SDM knowledge improved but there were no statistically significant changes in attitudes. Few self-reported behaviors differed post-intervention but more faculty reported that they would share different options for treating the medical condition. [Table] Preferred decision-making style did not differ with the majority choosing SDM both pre- and post-intervention (66% vs. 70% respectively, p=0.39). Over the 5-month post-intervention follow up period, 68% of faculty reported using a PDA tool in clinical practice with 32% using them >= 5 times.
Conclusion(s): Data suggests a multimodal educational intervention was effective at increasing PHM faculty SDM skills, knowledge and PDA utilization.
PHM faculty prefer synchronous educational activities for SDM.
.png)
.png)
