Neonatology
Session: Neonatal Quality Improvement 1
392 - Optimizing Neonatal Brain Development at a Level III NICU Through Participation in a Statewide Collaborative
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 392
Publication Number: 392.2125
Publication Number: 392.2125

Katherine Weiss, MD (she/her/hers)
Associate Professor of Pediatrics/Neonatology
University of California, San Diego School of Medicine
San Diego, California, United States
Presenting Author(s)
Background: Preterm infants are at high risk for altered brain development. Environmental stressors in the neonatal intensive care unit (NICU) impact this negatively. Positive parental touch (PPT), such as holding, skin-to-skin care (S2S), and hand hugs, has shown to have positive impact on short-term morbidities and long-term developmental outcomes and mortality. Despite the evidence supporting bonding, there is low parental engagement in NICU care in the United States due to multiple factors.
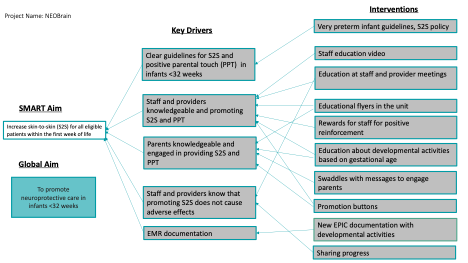
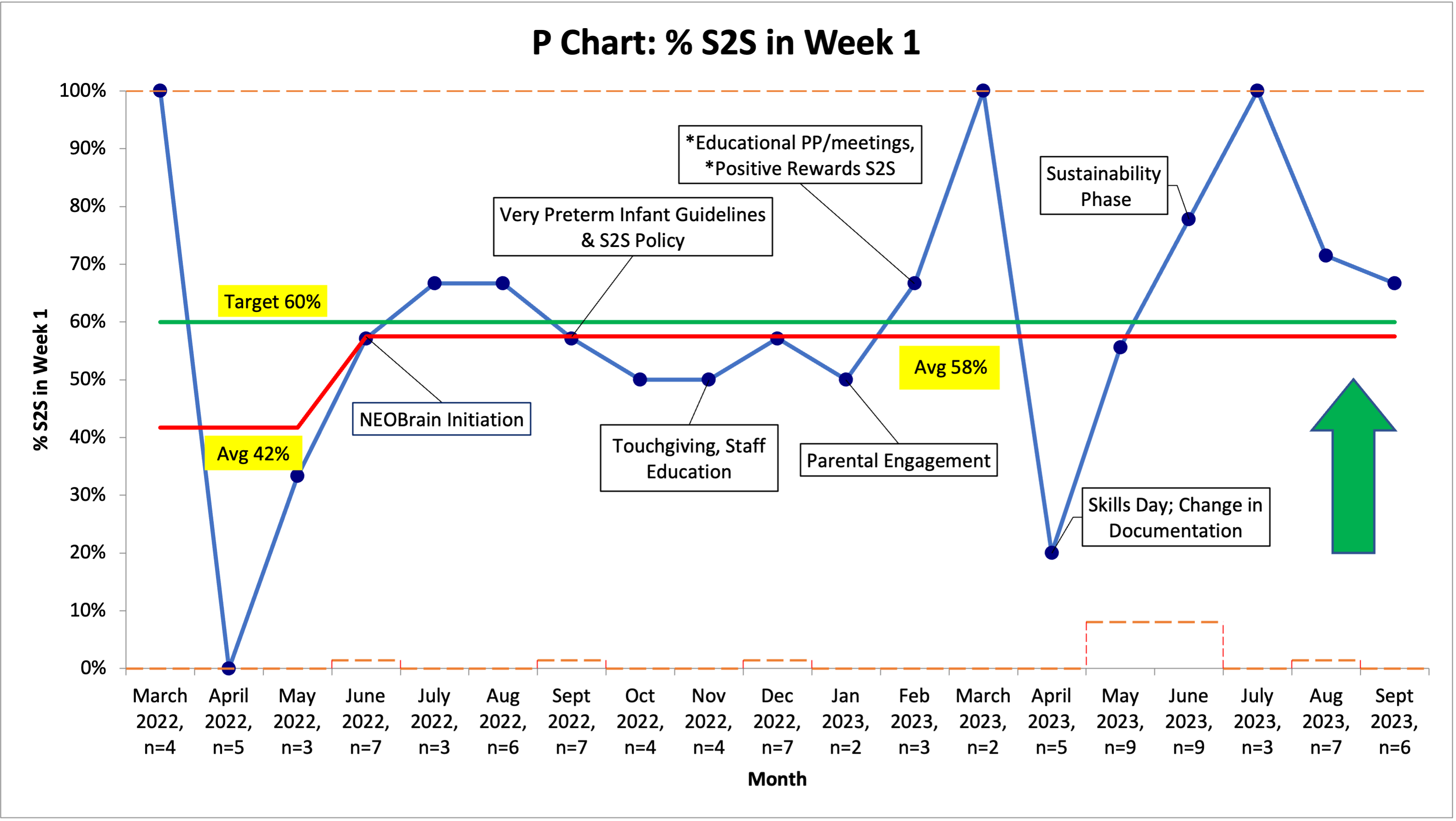
Objective: The primary aim is to increase S2S for all eligible patients within the 1st week of life by 40% from a baseline of 42% to a goal of 60% by May 31, 2023.
Design/Methods: University of California San Diego (UCSD) NICU is part of NICUs enabling optimal brain health (NEOBrain), a collaborative aimed at improving neuroprotective care in infants < 32 weeks of gestational age through the California Perinatal Quality Care Collaborative (CPQCC). The process measures were the percentage of patients who received S2S in the first 7 days of life, PPT in the first 72 hours and time to first S2S encounter. Balancing measures were unplanned extubation within the first 30 minutes of S2S transfer, unintentional line removal and severe IVH in the first 7-10 days of life. We updated our policy to opt more patients in to S2S and created educational materials to promote S2S and PPT in our NICU. Promotional items were created to sustain the gains. A multidisciplinary team of physicians, nurses, respiratory therapists, and occupational therapists provided education to the staff and providers. NICU parent liaisons were also included in the team to improve parental engagement.
Results: There was an increase in S2S in eligible infants within the first week of life from baseline 42% to 58% by May 2023 and continued improvement in sustainability phase. We have also achieved our secondary aims of establishing S2S in at least 25% extremely low birth weight (ELBW) infants within the first week of life and increasing PPT in 50% of eligible patients within the first 72 hours of life. There were no unplanned extubations or accidental line removals related to S2S. 7 of 84 subjects were noted to have severe IVH in the first 7-10 days of life but only 1 had S2S before the severe IVH was found.
Conclusion(s): Team effort and strategic planning can promote change in staff practices, increase parental engagement and potentially improve neuroprotective care and outcomes in the preterm population. Early S2S care and PPT has been shown to be a safe practice in our NICU.