Children with Chronic Conditions
Session: Children with Chronic Conditions 2
281 - Understanding Referral and Enrollment in a Pediatric Complex Care Program: Disparities & Predictors
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 281
Publication Number: 281.492
Publication Number: 281.492

Maria A. Schletzbaum, MD, PhD (she/her/hers)
Resident
St. Louis Children's Hospital
St. Louis, Missouri, United States
Presenting Author(s)
Background: Pediatric Complex Care Programs (PCCP) have emerged in the last 15 years to address the disproportionate health and service needs, economic impacts, and health services use that children with medical complexity (CMC) require. Amidst the high-intensity care coordination and medical co-management services PCCP deliver, little is known about their reach or whether they equitably serve CMC.
Objective: To evaluate characteristics of CMC who were eligible, referred to, and ultimately enrolled in a Pediatric Complex Care Program to identify potential disparities in PCCP access and uptake.
Design/Methods: This retrospective cohort study reviewed electronic health records data from a large Midwest health system between 2015-2021 to identify CMC ages 1-18 years meeting its PCCP eligibility criteria (≥3 specialists, ≥3 affected body systems, and either 5 hospital days or 10 clinic visits in a 1-year period). Eligible CMC were categorized as being referred (yes/no) and enrolled (yes/no) during this period. Statistically significant differences in eligible CMC referred vs non-referred, and enrolled vs non-enrolled were evaluated with multivariate logistic regressions adjusted for social and clinical confounders.
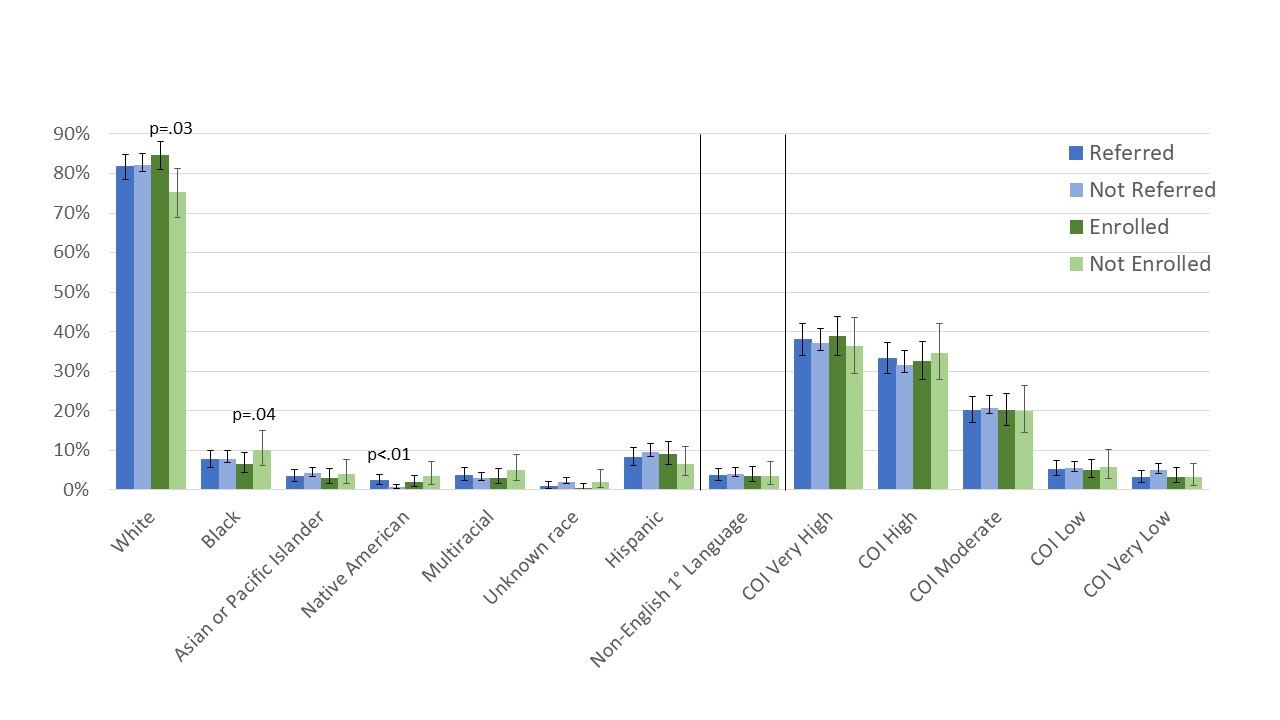
Results: Among 3,383 eligible CMC, 613 (18.1%) were referred and 414 (12.2%) enrolled. Figure 1 shows distributions of race/ethnicity, household language, and child opportunity index (COI) by referral and enrollment status. In adjusted analyses, there were no differences in referral or enrollment by child sex, primary language spoken, or COI (Figures 2 and 3). Referral was associated with younger age (aOR 0.95; 95% CI 0.93-0.97, per year of age), being Native American vs not (4.95; 2.26-10.84), having more ED visits (1.19; 1.07-1.33), inpatient days (1.006; 1.002-1.011), medications (1.05; 1.03-1.07), and specialists (1.40; 1.35-1.46), and fewer outpatient appointments (0.993; 0.990-0.996). Once referred, Black patients (0.52; 0.27-0.94 white patients) and those with more inpatient days were less likely to enroll (0.995; 0.986-0.999), while patients with more medications (1.04; 1.01-1.07) and specialists (1.10; 1.03-1.17) were more likely to enroll.
Conclusion(s): Referrals to PCCP have likely been occurring equitably for the included social factors; however, the enrollment disparity experienced by referred Black children requires attention. Opportunities exist to better understand and improve referral and enrollment patterns, e.g., many eligible CMC were never referred for complex care, and only two-thirds of eligible referrals resulted in enrollment.
.jpg)
.jpg)
