Neonatology
Session: Neonatal Quality Improvement 2
396 - Decreasing Time to Isolette Closure in a Neonatal Golden Hour Quality Improvement Initiative
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 396
Publication Number: 396.2128
Publication Number: 396.2128

Katherine Weiss, MD (she/her/hers)
Associate Professor of Pediatrics/Neonatology
University of California, San Diego School of Medicine
San Diego, California, United States
Presenting Author(s)
Background: The Golden Hour (GH) of neonatology is the hour immediately following birth in which fetal-neonatal transition is critical, especially for very premature infants. Medical care to prevent irreversible damage is most effective in this first hour. Protocols that prioritize the GH have been shown to improve short-term outcomes such as hypothermia, hypoglycemia, and timely initiation of fluids/medications, as well as long-term outcomes such as reducing rates of chronic lung disease, intraventricular hemorrhage, and retinopathy of prematurity. We are conducting a quality improvement project to optimize our Golden Hour (GH) for premature infants < 30 weeks in order to reduce their morbidity and mortality.
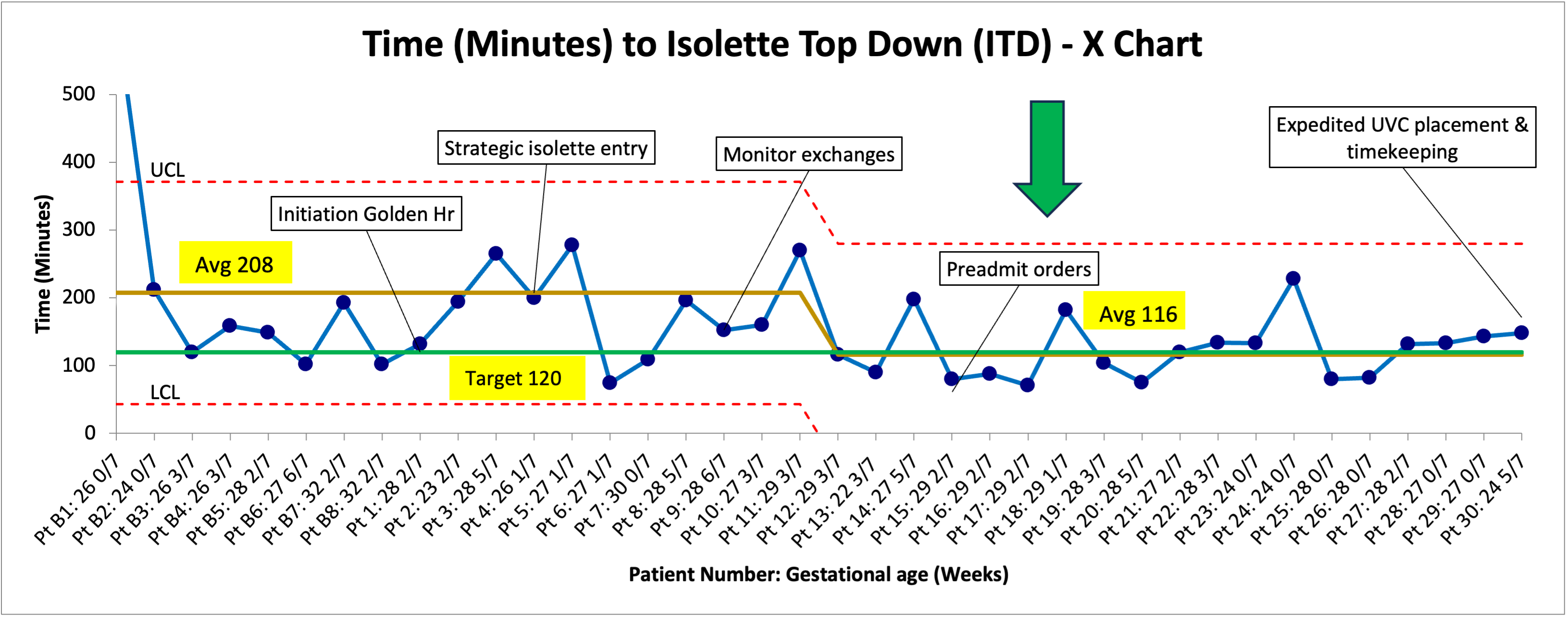
Objective: To decrease time to isolette top down (ITD), signaling the completion of Golden Hour, from 208 minutes to 120 minutes in preterm infants born < 30 weeks by December 31, 2023.
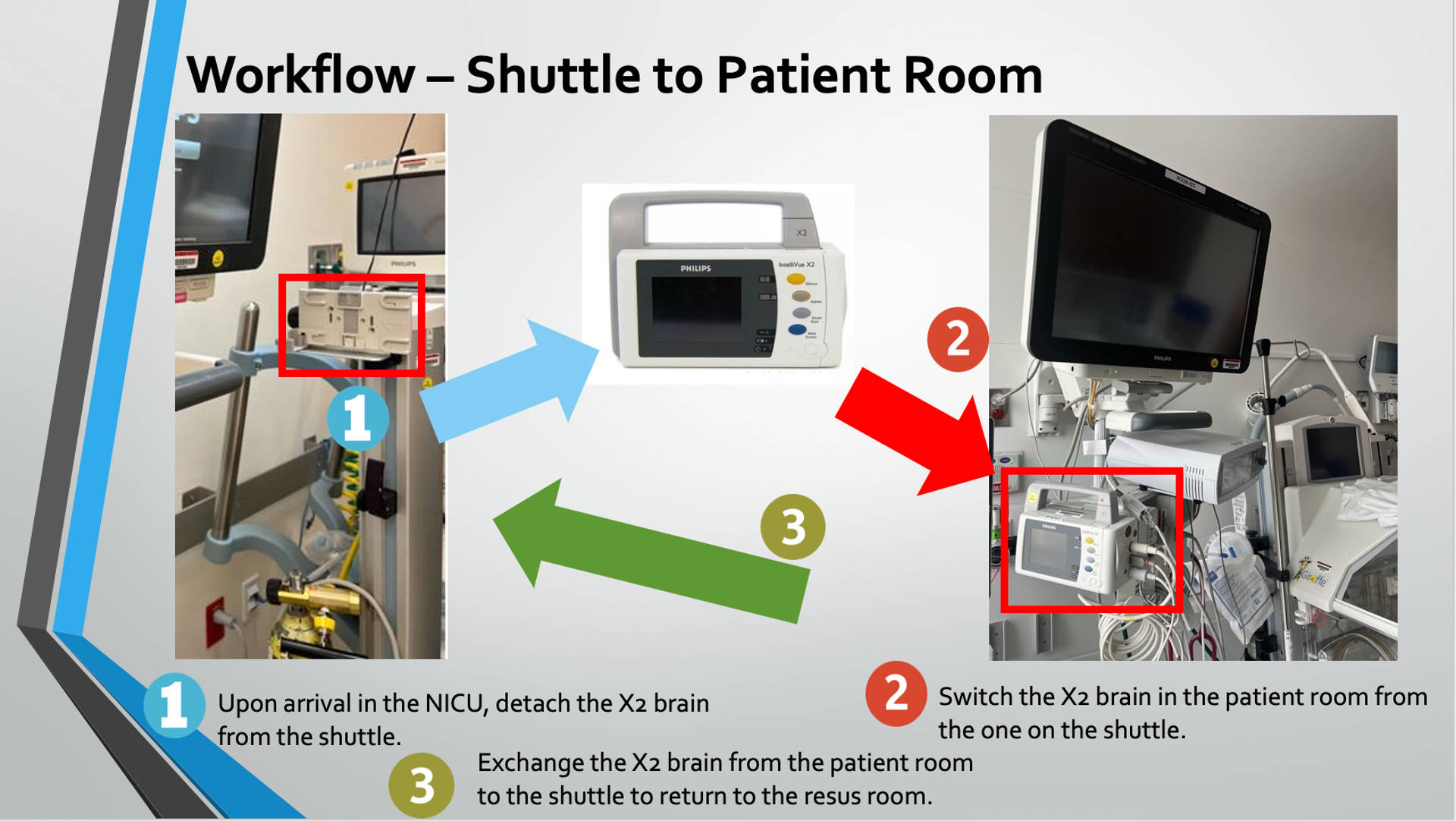
Design/Methods: The University of California San Diego NICU is a 52 bed Level 3 NICU with a birthing center that delivers approximately 40 infants with gestational age < 30 weeks per year. The care of these infants is standardized by the very preterm infant policy, updated in 2022. A multidisciplinary team of providers, nurses, respiratory therapists, pharmacists, radiology, and QI analysts met to implement and optimize the GH protocol. Baseline data showed an average of 208 minutes to ITD. A flowchart was created that assigned roles and tasks to the GH components. After a period of provider education, the initiative was implemented in January 2023. Several PDSA cycles have included strategic entry of the isolette to NICU room, monitor exchanges to ease the transport process, preadmit orders, and expedited initiation and timekeeping of umbilical venous catheter (UVC) placement. Data are reviewed monthly. Outcome measure is time to ITD. Process measures are time to NICU arrival from delivery room, time to initiation of UVC, and percent compliance to flowchart completion. Balancing measure is the burden of completing the flowchart.
Results: Since project initiation, the outcome measure of time to ITD decreased from a baseline of 208 minutes to 116 minutes. Time to start the UVC has shifted below the average and is being monitored with the recent goal of expedited UVC placement. Compliance with flowchart completion is 88%. Verbal and written feedback suggest no burden to flowchart completion.
Conclusion(s): Standardizing the very preterm GH with flowcharts and targeted innovative measures improved time to ITD and completion of the GH. We will continue to work for positive change through December 31, 2023 to ensure sustainability.