Neonatology
Session: Neonatal Follow-up 4
551 - Neurodevelopmental Outcomes after Neonatal Extracorporeal Membrane Oxygenation (ECMO)
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 551
Publication Number: 551.2889
Publication Number: 551.2889
- JN
Jaclynne H. Nader, MD (she/her/hers)
Resident
Hassenfeld Children's Hospital at NYU Langone
NY, New York, United States
Presenting Author(s)
Background: A standardized multifaceted approach to follow up is crucial for monitoring neurodevelopment in neonates who undergo extracorporeal membrane oxygenation (ECMO). The Pittsburgh Index for Pre-ECMO Risk plus (PIPER+) score, which predicts probability of hospital mortality, may help predict adverse neurodevelopmental outcomes.
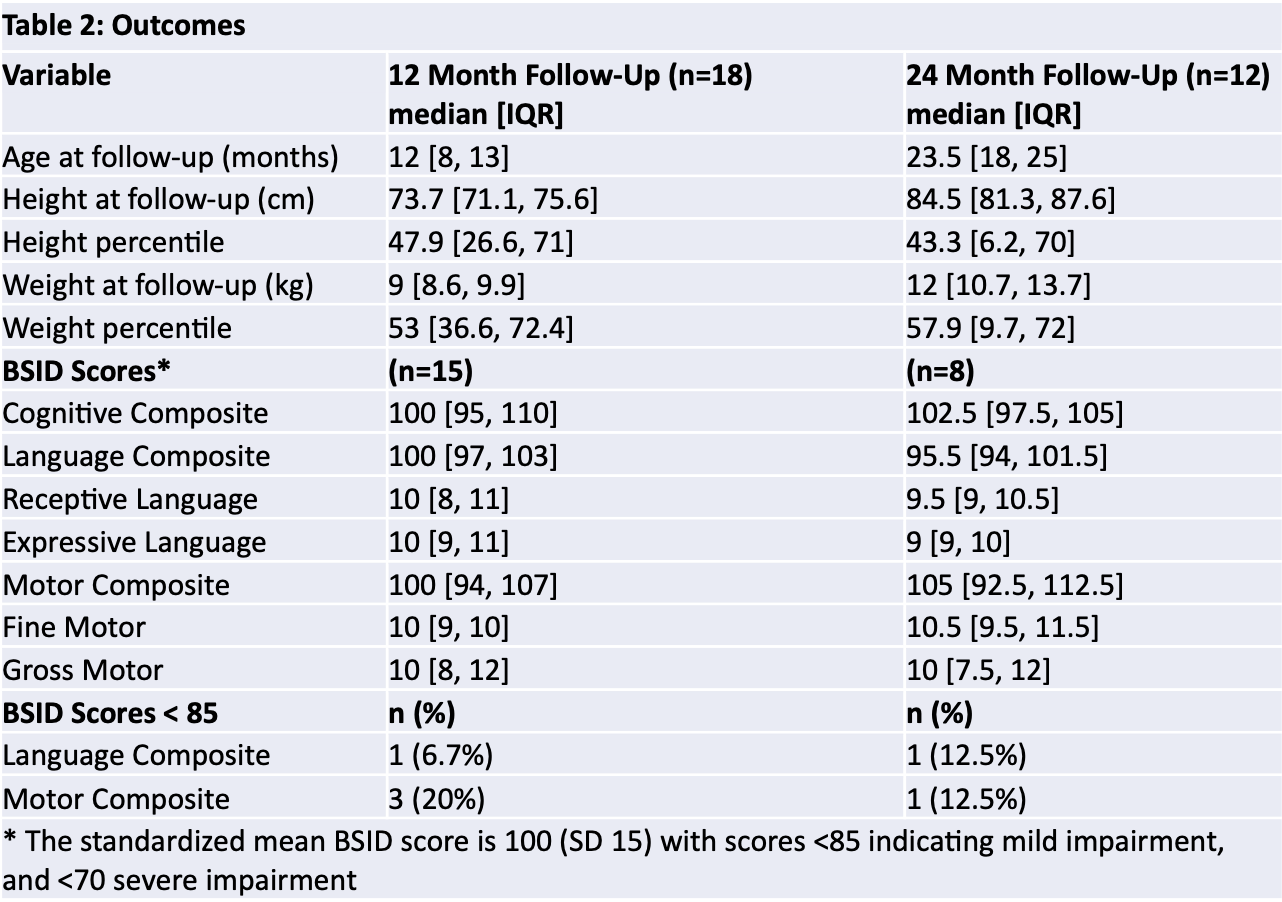
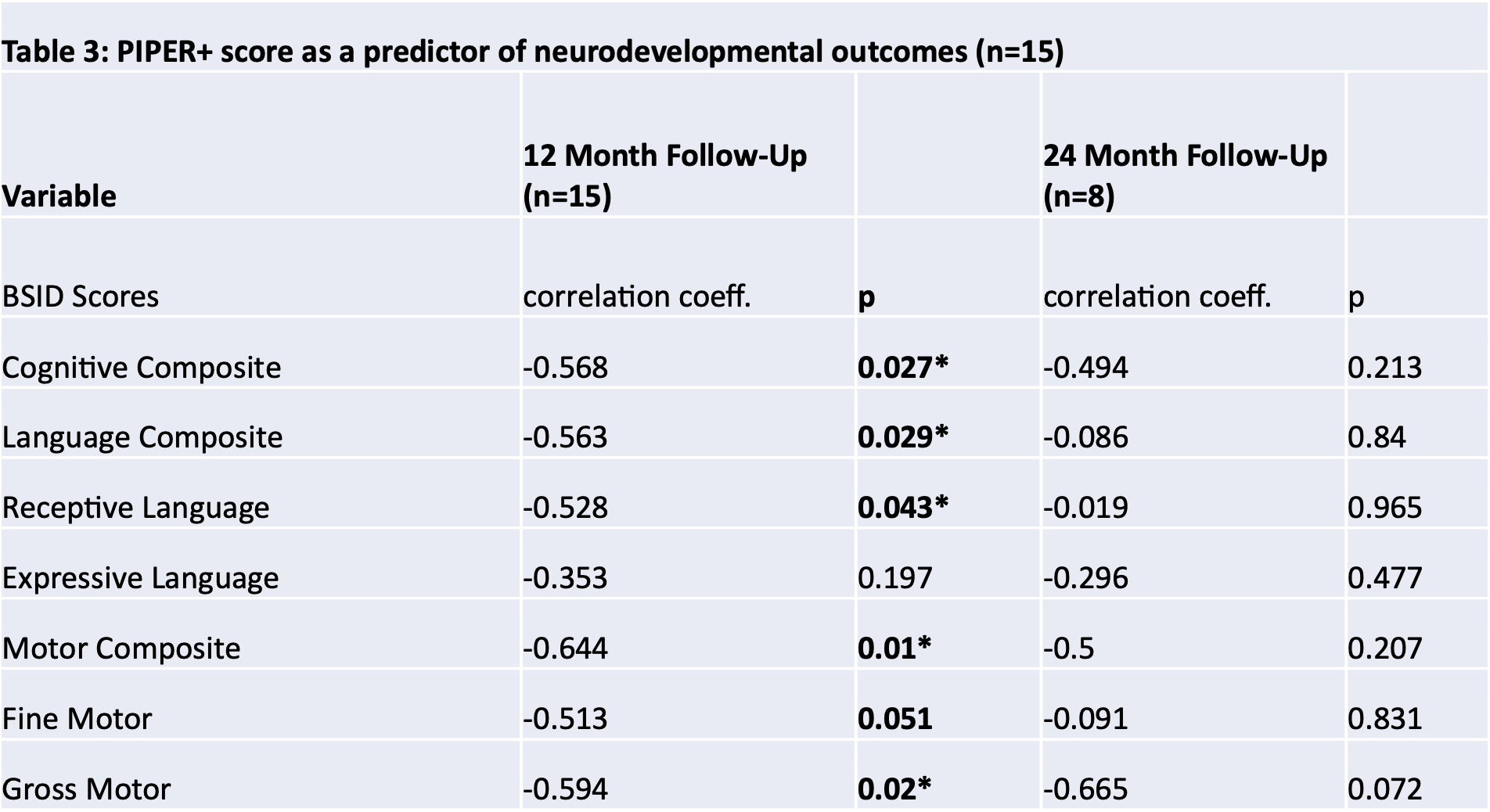
Objective: Assess neurodevelopment of neonates who were treated with ECMO in our new ECMO program, by analyzing Bayley Scales of Infant Development (BSID) scores obtained at our Neonatal Comprehensive Care Program (NCCP) clinic through 2 years of age. Determine whether neurodevelopmental outcomes in our study population were correlated to PIPER+ score, MRI or vEEG findings.
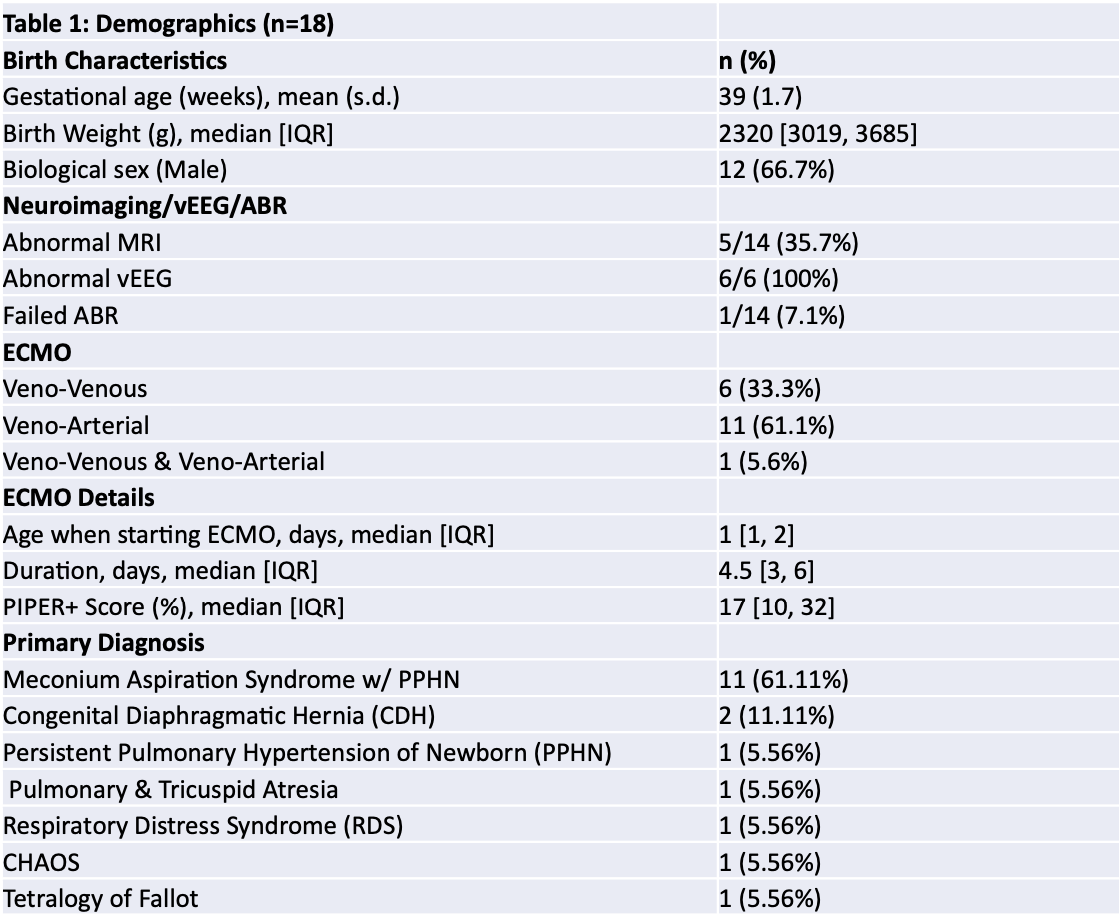
Design/Methods: We conducted a retrospective chart review of neonatal patients placed on ECMO at our institution between March 2015 and June 2023 who had at least one follow up visit at the NCCP clinic. The relationships between neurodevelopmental outcomes, quantified by the BSID score, PIPER + score, MRI results and vEEG abnormalities were analyzed.
Results: 18 patients met inclusion criteria. The primary diagnosis in the majority of patients was meconium aspiration (61%) followed by congenital diaphragmatic hernia (11.1%). At 12 months, mild impairments in language or motor (defined as BSID scores < 85) were seen in 6.7% and 20% of patients, respectively. At 24 months, mild impairments were seen in 12.5% of patients in each of the same domains. There was a significant negative correlation (p < 0.05) between PIPER+ and BSID scores at 12 months across all developmental domains analyzed. However, this correlation was no longer significant at 24 months. In our cohort, PIEPR+ score and 2-year mortality showed a significant correlation (OR 1.075, 95% CI 1.023-1.129). 14 patients underwent MRI, 5 of which were abnormal. 6 patients underwent vEEG, all of which were abnormal. Abnormal MRI or vEEG were not significantly correlated to worse BSID scores in any domains analyzed.
Conclusion(s): Neonatal ECMO survivors who were followed in our NCCP clinic did well, with very few children having BSID scores that were indicative of neurodevelopmental impairment. Higher PIPER+ scores were associated with mortality in our population as expected; furthermore, they were correlated with worse neurodevelopmental outcomes at 12 months. This correlation no longer existed at 24 months. Abnormal vEEG or MRI did not predict adverse neurodevelopmental outcomes in our population. It is important and feasible to follow neonates who underwent ECMO in a new ECMO program, using a pre-existing neurodevelopmental follow-up clinic.