Hospital Medicine
Session: Hospital Medicine 5
157 - Resource utilization and outcomes of single vs poly-viral bronchiolitis during and after the COVID19 pandemic across US children’s hospitals.
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 157
Publication Number: 157.1197
Publication Number: 157.1197
- CC
Clifford Chen, MD
Associate Professor
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Prior studies on poly-viral bronchiolitis were conducted before the COVID-19 pandemic and found little differences between poly-viral and single-virus bronchiolitis on severity of illness or resource utilization compared to single-viral bronchiolitis. Poly-viral testing increased with the COVID-19 pandemic allowing for the opportunity to examine the effects of poly-viral bronchiolitis on utilization and illness severity.
Objective: The objective was to compare resource utilization and clinical outcomes between patients admitted for single vs. poly-viral bronchiolitis.
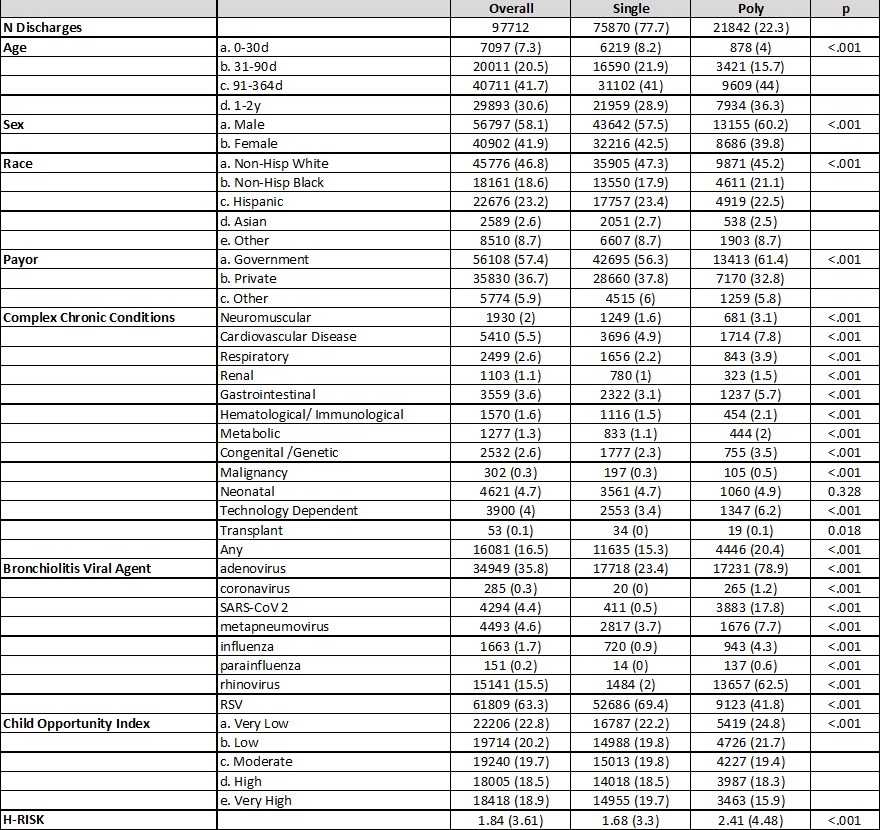
Design/Methods: Utilizing the Pediatric Health Information System (PHIS) database, we performed a retrospective cross-sectional study of children < 24 months discharged between 3/2020 and 3/2022 from children’s hospitals participating in the PHIS with a diagnosis code for bronchiolitis and at least one diagnosis code for a virus causing bronchiolitis. Encounters for bronchiolitis without a diagnosis code for virus-causing bronchiolitis were excluded. Single viral bronchiolitis encounters had one virus agent identified amongst the diagnosis codes, while poly-viral had 2 or more viruses. Between the 2 groups, we compared patient demographics, types of respiratory support, imaging, laboratory data, medications, ICU stay, and total length of stay (LOS) using chi-square and Wilcoxon-rank-sum in an unadjusted analysis. Additionally, compared outcomes adjusting for age, complex chronic conditions, payor, and hospital using generalized estimating equations.
Results: A total of 97,712 discharges met the inclusion criteria. 21842 (22.3%) were poly-viral encounters. Compared to single-virus bronchiolitis patients, poly-viral bronchiolitis patients were more likely to have a chronic complex condition (20.4% vs 15.3%). RSV was the most common virus found (63.3%) followed by adenovirus (35.8%). RSV was rarely co-infected with other viruses (14.8%). SARS CoV-2 prevalence was 4.4% and 90.7% of them were poly-viral.
In unadjusted analysis, patients with poly-viral bronchiolitis were more likely to utilize antibiotics (43% vs 36%), heated high-flow nasal cannula (32.3% vs 29.8%), non-invasive ventilation (12.1% vs 10.2%), invasive ventilation (11.4% vs 8%), ICU (38.5% vs 26%), and had a longer LOS (2.8 vs 2.5 days). In adjusted analysis, patients with poly-viral bronchiolitis were more likely to utilize the ICU (aOR 1.73, 95% CI 1.47-2.03) and have a longer LOS (aOR 1.2, 95% CI 1.15-1.26).
Conclusion(s): Encounters with poly-viral bronchiolitis had higher utilization of resources, more frequent ICU stays, and longer LOS compared to single virus bronchiolitis.
PAS abstract image 1.jpeg
PAS abstract image 3.jpeg
