Children with Chronic Conditions
Session: Children with Chronic Conditions 3
295 - Past and Current Care Practices for Neonates with Complex Medical Needs: A Scoping Review to support Clinical Program evaluation
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 295
Publication Number: 295.520
Publication Number: 295.520

Nicole Loewen, BSc
Graduate Research Assistant
University of British Columbia Faculty of Medicine
Vancouver, British Columbia, Canada
Presenting Author(s)
Background: Neonates with complex medical needs (NCMN) are a growing patient population internationally. Although NCMN are a relatively small proportion of all Neonatal Intensive Care Unit (NICU) admissions, they are high healthcare utilizers. Since 2018, NCMN at our hospital have been cared for by the multidisciplinary Neonatal Complex Care Team (NCCT) in a dedicated, single-family room, patient area within the NICU. This new model of care has not yet been evaluated for its potential impact on healthcare outcomes.
Objective: The objective of the scoping review is to determine the breadth of available literature on the care practices for management of NCMN and to collate the available evidence to define outcome measures to be used in a formal program evaluation.
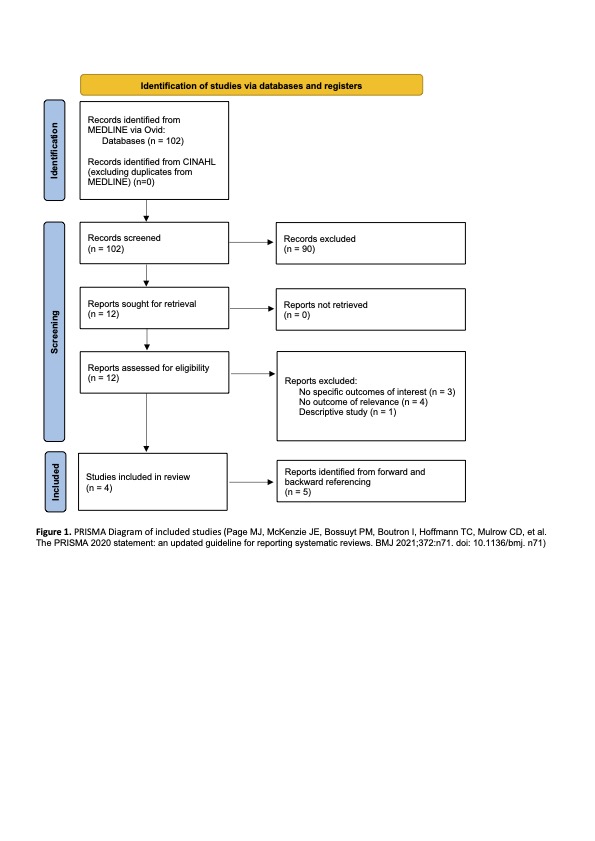
Design/Methods: The scoping review followed the PRISMA extension for scoping reviews and utilized resources from the Joanna Briggs Institute. The two databases that were utilized include Medline via OVID and CINAHL. The dates for inclusion are January 1st 1993, until July 15th 2023. Only studies published in English and primary research were included. Two independent reviewers performed the initial title and abstract screening, and the full text review. One reviewer completed the data extraction.
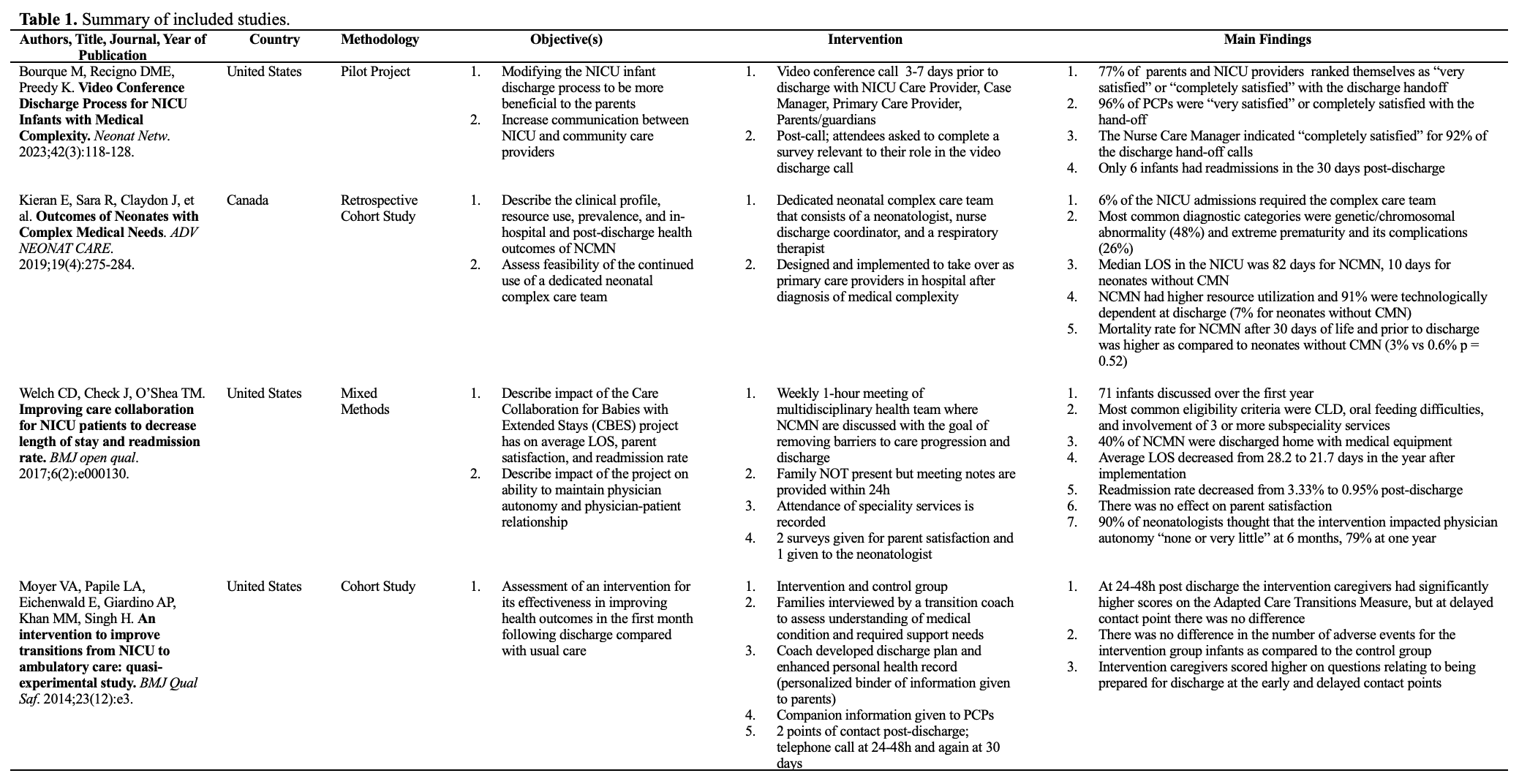
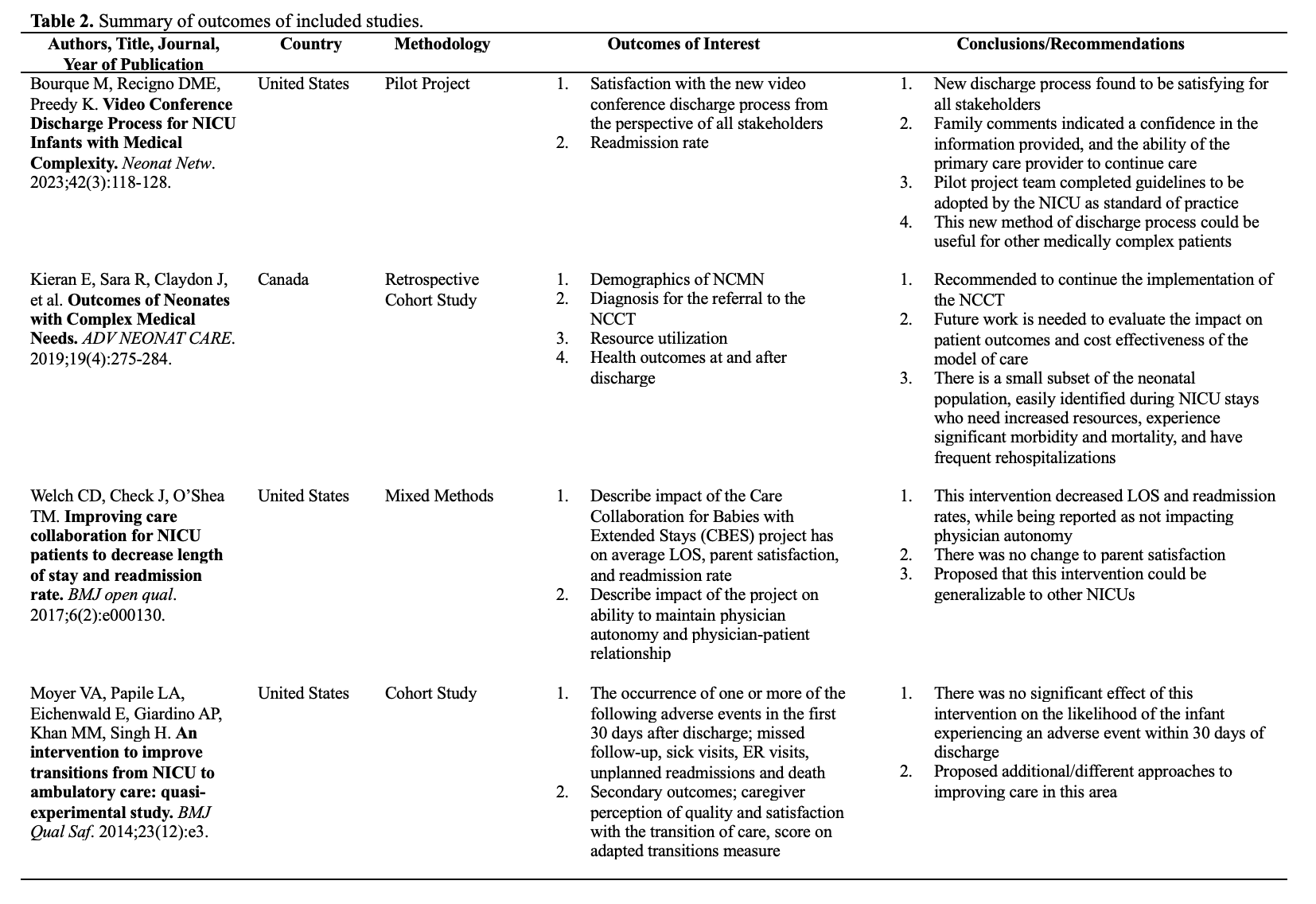
Results: 102 articles were included in the title and abstract screen, and 12 went for full text review. Ultimately, 4 articles were included (figure 1). The interventions discussed in the included articles ranged from discharge conferences with patient’s caregivers, to the implementation of an entirely new model of inpatient care (table 1). Multidisciplinary health care teams appear to be integral to the in-hospital care and smooth discharge of NCMN. Caregiver involvement and satisfaction are important to the discharge process as they are primarily responsible for their infant’s care when they leave the hospital, and so it is important that the specifics of care are communicated and taught effectively. The outcomes of interest identified as most useful for clinical program evaluation were length of stay and readmission rate (table 2). Additionally there was limited data reported on long-term health outcomes of this patient population.
Conclusion(s): This scoping review identified few articles that reported new models of care, a lack of consistent outcomes used in evaluating existing models and overall a gap in research in this rapidly growing patient population. There is more work to be done to improve care of NCMN and these findings will be used when designing future studies that evaluate novel models of care.