Nephrology
Session: Nephrology 3
5 - Correlation Between Ionized and Total Magnesium In Children On Continuous Renal Replacement Therapy
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 5
Publication Number: 5.2149
Publication Number: 5.2149

Shruthi Mohan, MBBS, MD (she/her/hers)
Pediatric nephrology fellow, PGY5
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Hypomagnesemia is associated with poor outcomes, including increased mortality. Regional citrate anticoagulation (RCA) during continuous renal replacement therapy (CRRT) can enhance the risk of hypomagnesemia in critically ill children, since citrate chelates divalent ionized magnesium (iMg) similar to ionized calcium (iCa), potentially leading to negative magnesium (Mg) balance. However, data regarding iMg in critically ill children undergoing CRRT is lacking. Existing data regarding the concordance between ionized and total magnesium levels (tMg) are conflicting. We hypothesized a weak correlation between iMg and tMg concentrations in children on CRRT receiving RCA, and a stronger correlation between iCa and iMg.
Objective: We aimed to correlate iMg with tMg/iCa in critically ill children before and during CRRT.
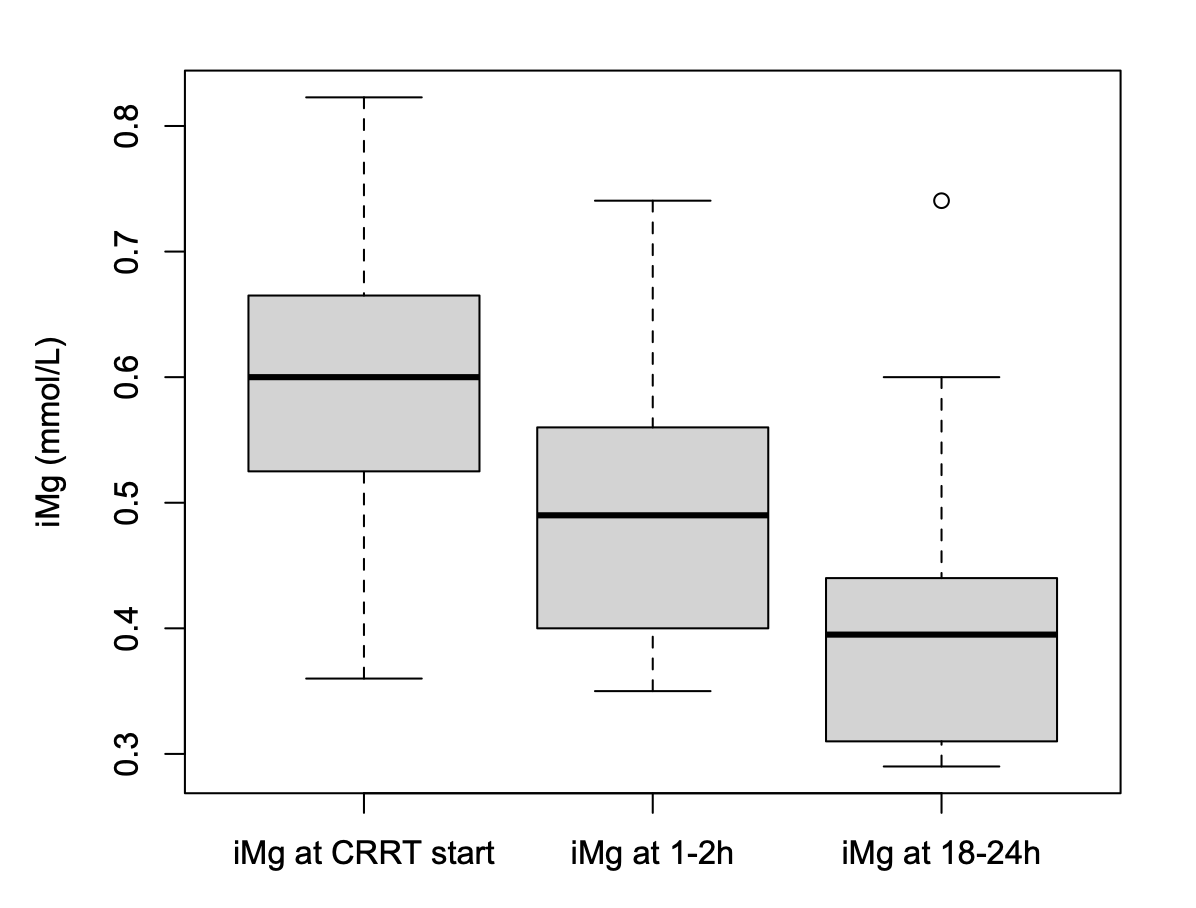
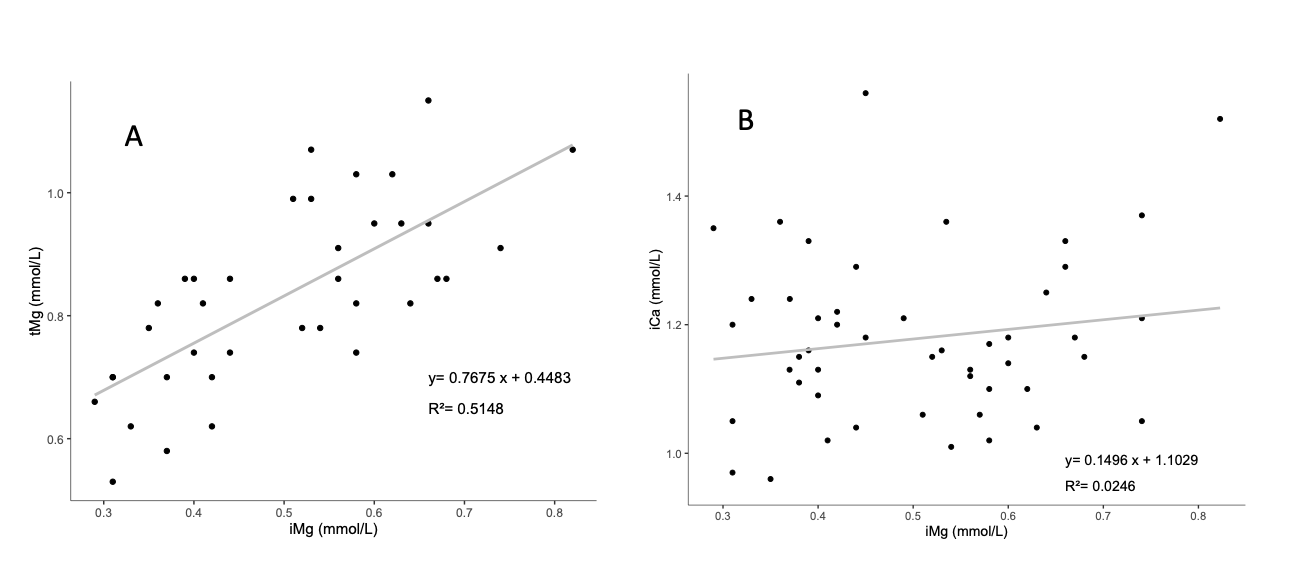
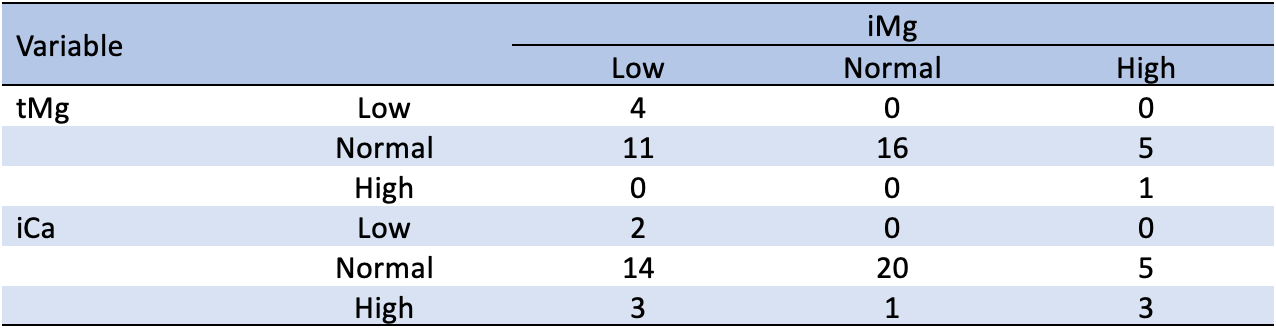
Design/Methods: We prospectively collected blood samples before, 1-2, and 18-24 hours after the initiation of a new CRRT circuit over a period of 1 year to measure iMg. We utilized tMg and iCa levels obtained for clinical purposes. Reference ranges of iMg, tMg and iCa concentrations of 0.44-0.65, 0.66-1.07 and 1.0-1.3 mmol/L, respectively, were considered normal. Linear mixed effect model was used to show the iMg trend after CRRT initiation. Fisher’s exact test and Cohen’s Kappa statistics were used for category agreement assessments. Pearson’s correlation coefficients and linear regression measured correlations.
Results: 17 patients were enrolled (N=48 iMg, N=37 tMg, N=49 iCa samples). 12% (N=2/17) of the patients had ionized hypomagnesemia at CRRT start. Subsequently, the percentage of patients with ionized hypomagnesemia increased to 35% (N=6/17), and 70% (N=12/17) at 1-2, and 18-24 hours after CRRT initiation respectively. A significant, progressive decrease in iMg was observed over time (Coefficient = - 0.005, p < 0.001). iMg and tMg (N= 37) were correlated (r = 0.71, p < 0.0001) and demonstrated category (low, normal, high) agreement (p = 0.019). Contrarily, iMg and iCa (N=48) did not correlate (r = 0.15, p = 0.28) or show category agreement (p = 0.069). Within 24 hours of CRRT onset, 24% of the patients (N=4/17) had additional Mg added to their TPN regimen compared to their baseline, and 6% (N=1/17) received a Mg bolus.
Conclusion(s): Our study revealed a strong correlation between iMg and tMg in critically ill children undergoing CRRT, but not with iCa. The prominence of ionized hypomagnesemia within 24 hours of CRRT initiation highlights the need for vigilant magnesium monitoring. These findings can guide further research on magnesium management in pediatric CRRT.